Laparoscopic cholecystectomy with only two 5 mm trocars in a pregnant woman with biliary pancreatitis
Introduction
Laparoscopic cholecystectomy (LC) is one of the most common surgeries performed. Historically, cholecystitis during pregnancy was managed non operatively with diet for chronic cholecystitis and antibiotics for acute cholecystitis (1). However, multiple reports emphasize that LC may be performed safely during pregnancy and seems superior to open cholecystectomy (2-6). Each trimester has its unique issues including teratogenic risk during early pregnancy, induction of labor during 2nd trimester with poor survival chances for the baby or severe complications (1,2). During advanced pregnancy the procedure is challenging due to the limited intraabdominal space. In contrast to cholecystitis, in case of biliary pancreatitis, removal of the gallbladder during the admission is still recommended in order to avoid repeat stone passage with possible severe complications especially during pregnancy (7,8).
In addition to the perioperative risk for mother and baby, patients may be at increased risk for developing a trocar site hernia due to the increasing intraabdominal pressure and significant mechanical stress on the incision during the birth act. Although no prospective studies on this issue are available, it seems reasonable to attempt to keep incisions for abdominal surgery as small as possible during pregnancy in order to reduce the risk for development of incisional hernias. We previously reported on a standard three port LC technique with placement of trocars in the left upper quadrant (LUQ). In addition we demonstrated that one port may be replaced by the Teleflex minigrasper even in more complex cases.
We report on a LC in a pregnant woman with biliary pancreatitis. Only two 5mm trocars and a Teleflex minigrasper were used. The specimen was removed through the LUQ port site.
Case presentation
A 35-year-old Hispanic female in her 22nd week of pregnancy came to the emergency room (ER) with acute right upper quadrant pain. Due to lack of accessibility she had poor prenatal care. She had mildly elevated amylase but normal LFTs and ultrasound showed some gallbladder wall thickening suggestive for acute cholecystitis but no dilated extra and intrahepatic biliary duct system was observed. Fetal ultrasound was normal. She was admitted to the hospital and started on antibiotics, obstetrics was consulted. Her amylase peaked at >600 U/L after three days but then normalized and indication for LC was made. MRCP and ERCP were not performed as it was assumed that the patient had passed a stone and during consent she was informed that due to her pregnancy an intraoperative cholangiography (IOC) would be avoided but she would have to remain hospitalized for few days to trend her LFTs and lipase/amylase. Also her baby would be monitored.
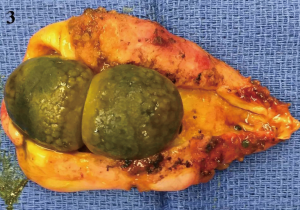
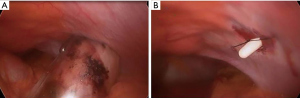
She was brought to the OR and was anaesthetized. Five mm trocars were placed in the LUQ and the umbilicus and a Teleflex minigrasper was inserted between the two ports. The uterus was found at the umbilical level (Figure 1A). The GB was pulled out and the serosa was incised on both sides close to the liver rim (Figure 1B) and a window was created behind the GB midportion and widened towards infundibulum and fundus (Figure 1C). GB wall thickening and edema were found. The critical view was obtained and the cystic artery and duct were clipped and divided (Figure 1D). The common bile duct appeared normal and as planned no IOC was done. The specimen was retrieved through the LUQ port site using a 5 mm endobag after dilatation to 12 mm due to the presence of two large stones (Figure 2A). The port site fascia was closed using a suture passer (Figure 2B). The gallbladder contained two 1 cm stones and multiple smaller stones (Figure 3).

The postoperative course was uneventful and the patient was discharged on postoperative day two after fetal ultrasound confirmed no complications. Both mother and baby were well during follow up; a vaginal delivery was done. There was no evidence for development of an incisional hernia during follow up.
Discussion
We report on a “microinvasive” LC during pregnancy. We previously reported a large series of LCs using a 3 instrument approach and for uncomplicated cases the Teleflex minigrasper was found to be able to completely replace a trocar based 5 mm grasper (9-11). In subsets of patients including those with biliary dyskinesia and cholecystitis due to sludge or small stones only two five mm trocars are necessary.
In pregnant women, replacing a 10–12 mm trocar by a 5 mm trocar may help prevent a trocar site hernia. However, we still had to spread the extraction site to 12 mm as the GB contained two large stones. Conclusive data on trocar hernias in this patient population are not available. We believe our approach with extraction of the specimen through the LUQ port site may have some advantages over the umbilical extraction. This approach with the smallest possible incisions and fewest instruments seems in pregnant women desirable and may be less invasive than the recently suggested single port approach with a relatively large umbilical incision (12). Due to the limited intraabdominal space, an approach from the LUQ also seems to have advantages avoiding unnecessary “sword fighting” with laparoscopic instruments.
When using a three instrument technique, some adaptations to the dissection need to made. Instead of isolating the cystic artery and duct first, clipping and dividing them and then dissecting the GB out, we suggest a modified dome down technique. We first created a window behind the GB and pulled the GB out, which requires only one grasper. Once the window is widened towards the infundibulum, CD and CA stretch out and can be easily isolated and the critical view is easily obtained. We leave the GB suspended at the fundus with a small tissue band, which allows traction and counter-traction as opposed to the classic dome down technique.
In case of biliary pancreatitis during pregnancy, LC should be performed during first admission as repeat stone passage could lead to significant complications (7,8). If ultrasound shows a normal biliary system and amylase/lipase normalize such as in our case, MRCP/ERCP and IOC may be avoidable to protect the baby. If there is any evidence for choledocholithiasis, an ERCP seems the best approach followed by LC.
To summarize, LC with two ports is feasible during pregnancy. The Teleflex needle grasper is able to completely replace a trocar based grasper. Removal of the specimen through a lateral abdominal wall site may help prevent an umbilical port site hernia in this patient population.
Acknowledgments
Parts of this work were presented at SAGES 2018.
Funding: None.
Footnote
Conflicts of Interest: The author has completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ls.2018.10.05). The author has no conflicts of interest to declare.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Declaration of Helsinki (as revised in 2013). The patient was lost to follow up and no identifiable characteristics of the patient were given.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Hedstrom J, Nilsson J, Andersson R, et al. Changing management of gallstone-related disease in pregnancy - a retrospective cohort analysis. Scand J Gastroenterol 2017;52:1016-21. [PubMed]
- Athwal R, Bhogal RH, Hodson J, et al. Surgery for gallstone disease during pregnancy does not increase fetal or maternal mortality: a meta-analysis. Hepatobiliary Surg Nutr 2016;5:53-7. [PubMed]
- Cox TC, Huntington CR, Blair LJ, et al. Laparoscopic appendectomy and cholecystectomy versus open: a study in 1999 pregnant patients. Surg Endosc 2016;30:593-602. [Crossref] [PubMed]
- Nasioudis D, Tsilimigras D, Economopoulos KP. Laparoscopic cholecystectomy during pregnancy: A systematic review of 590 patients. Int J Surg 2016;27:165-75. [Crossref] [PubMed]
- Sedaghat N, Cao AM, Eslick GD, et al. Laparoscopic versus open cholecystectomy in pregnancy: a systematic review and meta-analysis. Surg Endosc 2017;31:673-9. [Crossref] [PubMed]
- Paramanathan A, Walsh SZ, Zhou J, et al. Laparoscopic cholecystectomy in pregnancy: An Australian retrospective cohort study. Int J Surg 2015;18:220-3. [Crossref] [PubMed]
- Ducarme G, Maire F, Chatel P, et al. Acute pancreatitis during pregnancy: a review. J Perinatol 2014;34:87-94. [Crossref] [PubMed]
- Yang DJ, Lu HM, Guo Q, et al. Timing of Laparoscopic Cholecystectomy After Mild Biliary Pancreatitis: A Systematic Review and Meta-Analysis. J Laparoendosc Adv Surg Tech A 2018;28:379-88. [Crossref] [PubMed]
- Bonatti H, Fisher MJ. Combined laparoscopic cholecystectomy and deroofing of a large liver cyst with a two trocar technique and use of a needle grasper. Eur Surg 2017;49:288-92. [Crossref]
- Bonatti H, Fisher MJ, Taskin V. Hybrid laparoscopic cholecystectomy and ERCP - a rational approach to choledocholithiasis. Eur Surg 2017;49:S1-115.
- Bonatti H. Three port cholecystectomy with a modified dome down technique - a safer and more ergonomic way to do it? Eur Surg 2016;48:1-112.
- Behera RR, Salgaonkar HP, Bhandarkar DS, et al. Laparoendoscopic single-site cholecystectomy in a pregnant patient. J Minim Access Surg 2013;9:183-6. [Crossref] [PubMed]
Cite this article as: Bonatti H. Laparoscopic cholecystectomy with only two 5 mm trocars in a pregnant woman with biliary pancreatitis. Laparosc Surg 2018;2:55.