
Effect of position and pneumoperitoneum on respiratory mechanics and transpulmonary pressure during laparoscopic surgery
Introduction
Optimizing mechanical ventilation during laparoscopic surgery may potentially improve gas exchange, minimize alveolar collapse and atelectasis and protect the lungs.
Evaluation of esophageal pressure, which correlates closely with pleural pressure (Ppl), enables good estimation of transpulmonary pressure (TPP), which could in turn assist in determining required positive end expiratory pressure (PEEP) in ventilated patients (1).
Airway pressure is a poor indicator of lung mechanics because it ignores the effect of chest wall compliance, which is affected by changeable conditions generated during various surgical procedures and in critical ill states.
Since esophageal pressure had been clinically used to optimize PEEP in various clinical settings (2-6), and to guide pulmonary protective ventilation strategy for a better management of acute lung injury (ALI) and acute respiratory distress syndrome (ARDS) (7), and to evaluate the effects of prone position on respiratory mechanics (8).
The influence of surgical positioning, as well as the pneumoperitoneum induced for laparoscopic surgery on respiratory mechanics has been evaluated (9), but their effect on esophageal pressure was not deeply studied. The present clinical trial was designed to measure and compare the effects of head up and head down positions, as well as various degrees of pneumoperitoneum on respiratory mechanics and esophageal pressure.
Methods
Patients and study design
The study was planned as a prospective observational study. Following approval by the Institutional Review Board, the study was performed in Rambam Healthcare Campus, Haifa, Israel—a university affiliated referral hospital. Patients scheduled for elective laparoscopic surgery aged between 20 and 60 years were included. Each participant signed an informed consent. Exclusion criteria included respiratory pathology, a body mass index lower than 18 or higher than 40 kg/m2, esophageal pathology and previous esophageal or pulmonary operation.
Following induction of anesthesia using fentanyl 2–5 microgram/kg, propofol 1–3 mg/kg and muscle relaxation with rocuronium 0.6–0.8 mg/kg, the trachea was intubated using a 7–8 mm ID cuffed endotracheal tube. Mechanical ventilation in a volume controlled mode with a tidal volume 8 mL/kg and a PEEP of 5 cm of water, Inspiratory to expiratory (I:E) ratio of 1:2 and 10% of plateau time was initiated at a rate of 12–16 breaths per minute using an anesthesia machine (Fabius GS Premium, Drägerwerk AG & Co. KGaA, Lübeck, Germany). Balanced general anesthesia was maintained by sevoflurane and fentanyl.
Physiological measurements
After confirmation of muscle relaxation using a nerve stimulator yielding a train of four (TOF) count of less than two, Esophageal balloon catheter was placed according to manufacturer instructions (10). The stomach was decompressed and suctioned with an 18 F orogastric tube. A designated esophageal pressure catheter (Adult Esophageal Balloon Catheter, Cooper Surgical, CT, USA) was inserted nasally and advanced into the lower third of the esophagus. The proximal ending of the catheter and connected to a syringe and a pre-calibrated pressure transducer via a 3-way stopcock. One ml of air was injected into the balloon so that it became semi inflated, and the tracing on the pressure monitor was adjusted with additional air until no flattening or damping was noted in the pressure waveform.
Esophageal pressure was continuously measured via a calibrated pressure transducer system (Art-Line, BioMetrix, Kiryat Mada, Jerusalem, Israel) connected to a patient monitor (Datex AS/3, Datex Ohmeda Medical Equipment, GE Healthcare, USA) and recorded using a designated computer software (11).
Esophageal pressure was documented with the head up 20 cm (anti Trendelenburg position), the patient at horizontal position, and with and head down 20 cm (Trendelenburg position).
Following peritoneal access and trocar insertion, the peritoneal cavity was gradually inflated with carbon dioxide by a laparoscopy insufflator (UHI-4 High Flow Insufflation Unit, Olympus Corporation Inc., Center Valley, PA, USA) and esophageal pressure was recorded at a stable peritoneal pressure of 5, 10 and 15 mmHg. Following complete peritoneal inflation, the esophageal balloon catheter was removed and recording terminated.
Statistical analysis
Statistical analysis was conducted by SPSS version 21 (SPSS, IBM, Chicago, IL, USA). Descriptive statistics in terms of mean, SD, median and percentiles were demonstrated to all parameters in the study. Normal distributions of the quantitative parameters were examined by Kolmogorov-Smirnov test, and parametric or non-parametric tests were used as appropriate (i.e., non-parametric tests were used for variables with other than normal distribution).
Results
Twenty healthy patients were recruited as participants between May 31st 2018 and August 13th 2018, all of which have successfully completed all the study tasks. Their demographic data is presented in Table 1.
Table 1
| Demographics | Values |
|---|---|
| Gender (M/F) | 8/12 |
| Age (years) | 51.7±20 |
| Height (cm) | 165.8±7.2 |
| Weight (kg) | 73.2±13 |
| BMI (kg/cm2) | 26.6±5.1 |
Values are presented as mean ± standard deviation. BMI, body mass index.
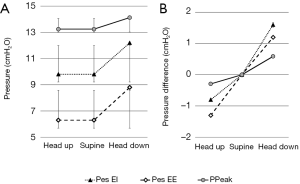
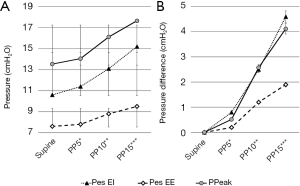
Peak airway pressure (PPeak), as well as end inspiratory and end expiratory esophageal pressures (Pes EI and Pes EE, respectively) were recorded during supine ventilation, head up and head down positions, and, following initiation of peritoneal cavity insufflation with carbon dioxide, supine position during pneumoperitoneum of 5, 10 and 15 mmHg.
The measured PPeak, calculated dynamic compliance, as well as measured Pes EI and Pes EE are presented in Table 2.
Table 2
| Position/intervention | PPeak¥ (cmH2O) | Compliance (mL/cmH2O) | Pes EI¥ (mmHg) | Pes EE¥ (mmHg) |
|---|---|---|---|---|
| Head up 15° | 18±2.5 (−0.4±2.7) | 44±7.3* | 9.8±3.8 (−1.3±2.8) | 6.3±2.4 (−1.7±3.1)* |
| Supine | 18.4±4.2 | 43.2±13.3 | 10.6±4 | 7.6±3.9 |
| Head down 15° | 19.2±4.2 (0.8±1.9) | 40.1±9.3 | 12.2±3.8 (1.6±1.6)*** | 8.8±4.2 (1.2±1.5)** |
| Pneumoperitoneum 5 cmH2O | 19.1±4.5 (0.7±3.1) | 42.6±11.9 | 11.4±4.3 (0.7±2.5) | 7.8±5 (0.1±2.1) |
| Pneumoperitoneum 10 cmH2O | 21.9±5.2 (3.4±3.7)*** | 33.4±6.5* | 13.1±4.3 (2.4±2.8)** | 8.8±5.1 (1.2±2)* |
| Pneumoperitoneum 15 cmH2O | 24±6.4 (5.5±4.5)*** | 30.6±8.7* | 15.2±5.8 (4.6±4.1)*** | 9.5±5.8 (1.9±2.9)** |
¥, values are presented as average ± standard deviation, with difference from supine baseline in brackets; *, P<0.05; **, P<0.01; ***, P≤0.001 Wilcoxon Signed-Rank Test compared to supine baseline. PPeak, peak airway pressure; Pes EI, end inspiratory esophageal pressure; Pes EE, end expiratory esophageal pressure.
As significant pressure and compliance variability exists between subjects, the difference between baseline (supine) pressures and each pressure measurement was calculated.
The PPeak and esophageal pressure difference from baseline is presented in brackets Table 2.
Mean PPeak, Pes EI and Pes EE during changes in position is presented in Figure 1A, and the change from baseline (supine) pressures is presented in Figure 1B.
Pressures during surgical pneumoperitoneum in increasing pressures are presented in Figure 2A, and the change from baseline (supine, no pneumoperitoneum) pressures is presented in Figure 2B.
Discussion
Pes is highly dependent upon body posture. Ideally, it is measured in an upright position, where the vertical gravitational axis is aligned with the general cephalocaudal direction of the esophagus. In the upright position, the horizontal forces acting on the air-filled balloon of esophageal catheter are mainly those transmitted from the surrounding structures of the chest. The intrapleural space lies at the closest proximity to the balloon and the pressure measured within it reflects Ppl applied to the surface of the lung (12,13). In the supine position, there is an additional pressure vector generated by the weight of mediastinal content that is perpendicular to the esophageal axis. It is termed mediastinal artifact and may increase Pes. Pes is not only influenced by the mediastinal artifact, but also by changes of intra-abdominal pressure as the result of a cephalad movement of the diaphragm. An early study conducted in patients with tuberculosis and in whom the pleural and esophageal pressures were recorded simultaneously, demonstrated significant larger amplitude variability and greater absolute positive pressure values in a supine, compared to upright position (14). In a subsequent study, a smaller effect was found with posture changes from upright to supine (15). More recent data show an increased Pes of few cmH2O in the supine compared to upright position (16,17).
Pes is not only influenced by the mediastinal artifact, but also by changes of intra-abdominal pressure producing an additional force transmitted to the relatively compliable mediastinum. Intra-abdominal pressure of 5 to 7 mmHg is considered normal. However, such normal range is not applicable for all. Morbidly obese and pregnant individuals can have chronically elevated intra-abdominal pressure (as high as 10 to 15 mmHg) without adverse sequelae (18). Intra-abdominal hypertension is defined as grade I at a pressure of 12 to 15 mmHg and grade IV at pressures exceeding 25 mmHg. Abdominal compartment syndrome with impaired perfusion and function of nearly every organ system is defined as a sustained intra-abdominal pressure greater than 20 mmHg (19). Nevertheless, intra-abdominal pressure of 25 mmHg may not always result in abdominal compartment syndrome since its actual development depends upon individual variables such as blood pressure, chronicity of the causative process and abdominal wall compliance (20). Although we have shown in this study that the changes in Pes correlated well with PPeak, the changes in Pes appeared a phase earlier (already a 5 mmHg, Figure 1). Certainly Pes should not be utilized as monovalent sign for this purpose since it depends on many variables including obesity (17) which by itself might produce increased intra-abdominal pressure, but it can be added as an additional parameter for early warning to the development of intra-abdominal hypertension.
The use of esophageal pressure monitoring is no longer confined to a handful of enthusiasts, scientists and clinicians. Some 70 years after being first invented by a doctoral student in 1949 who showed the possibility to use esophageal pressure as a surrogate for Ppl, it has become an increasingly common method for intensive care patients and for those who are in a critical condition under anesthesia. Such progress was achieved as a result of a better understanding of the capabilities and limitations of the method, the standardization of the equipment used for monitoring and the insertion technique of the probe and its proper location in the esophageal lumen (2). Despite the accumulated knowledge, there are still open issues, some of which have been examined in this study—the effect of moderate head up—head down (Trendelenburg) positions and elevated intra-abdominal pressure during laparoscopy on esophageal pressure. A moderate (15°) head-up position slightly reduced both, end-expiratory and end-inspiratory esophageal pressures whereas similar degree of head-down elevated these two esophageal pressures. In contrast, intra-abdominal pressure of 10–15 mmHg increased both, end-expiratory and end-inspiratory esophageal pressures. This intra-abdominal pressure is achieved during gas insufflation into the abdomen to create pneumoperitoneum for most standard surgical laparoscopic procedure (21).
Conclusions
This study shows that both moderate posture changes and pneumoperitoneum, significantly elevated esophageal pressure as well as airway pressure. These findings could be relevant to patients in extreme conditions and mechanical ventilation for them should better be assisted by Pes monitoring. High PEEP (possibly greater than 10 cm of water) may be required to compensate for the increase in TPP when performing laparoscopic surgery requiring high pressures or extreme head down position.
Acknowledgments
Funding: The study was supported by the Department of Anesthesiology, Rambam Health Care Campus.
Footnote
Conflicts of Interest: The authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ls.2018.10.13). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Institutional Review Board of Rambam Healthcare Campus and each participant signed an informed consent.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Santa Cruz R, Rojas JI, Nervi R, et al. High versus low positive end-expiratory pressure (PEEP) levels for mechanically ventilated adult patients with acute lung injury and acute respiratory distress syndrome. Cochrane Database Syst Rev 2013;CD009098 [PubMed]
- Akoumianaki E, Maggiore SM, Valenza F, et al. The application of esophageal pressure measurement in patients with respiratory failure. Am J Respir Crit Care Med 2014;189:520-31. [Crossref] [PubMed]
- Fish E, Novack V, Banner-Goodspeed VM, et al. The Esophageal Pressure-Guided Ventilation 2 (EPVent2) trial protocol: a multicentre, randomised clinical trial of mechanical ventilation guided by transpulmonary pressure. BMJ Open 2014;4:e006356 [Crossref] [PubMed]
- Talmor D, Sarge T, Malhotra A, et al. Mechanical ventilation guided by esophageal pressure in acute lung injury. N Engl J Med 2008;359:2095-104. [Crossref] [PubMed]
- Talmor D, Sarge T, O'Donnell CR, et al. Esophageal and transpulmonary pressures in acute respiratory failure. Crit Care Med 2006;34:1389-94. [Crossref] [PubMed]
- Talmor DS, Fessler HE. Are esophageal pressure measurements important in clinical decision-making in mechanically ventilated patients? Respir Care 2010;55:162-72; discussion 172-4. [PubMed]
- Mietto C, Malbrain ML, Chiumello D. Transpulmonary pressure monitoring during mechanical ventilation: a bench-to-bedside review. Anaesthesiol Intensive Ther 2015;47:s27-37. [Crossref] [PubMed]
- Kumaresan A, Gerber R, Mueller A, et al. Effects of Prone Positioning on Transpulmonary Pressures and End-expiratory Volumes in Patients without Lung Disease. Anesthesiology 2018;128:1187-92. [Crossref] [PubMed]
- Valenza F, Vagginelli F, Tiby A, et al. Effects of the beach chair position, positive end-expiratory pressure, and pneumoperitoneum on respiratory function in morbidly obese patients during anesthesia and paralysis. Anesthesiology 2007;107:725-32. [Crossref] [PubMed]
- CooperSurgical CDT, CT 06611 USA. 47-9005 • Adult Esophageal Balloon Catheter Directions for Use (English), 2014.
- Lee HC, Jung CW. Vital Recorder-a free research tool for automatic recording of high-resolution time-synchronised physiological data from multiple anaesthesia devices. Sci Rep 2018;8:1527. [Crossref] [PubMed]
- Cortes GA, Marini JJ. Two steps forward in bedside monitoring of lung mechanics: transpulmonary pressure and lung volume. Crit Care 2013;17:219. [Crossref] [PubMed]
- Sahetya SK, Brower RG. The promises and problems of transpulmonary pressure measurements in acute respiratory distress syndrome. Curr Opin Crit Care 2016;22:7-13. [Crossref] [PubMed]
- Mead J, Gaensler EA. Esophageal and pleural pressures in man, upright and supine. J Appl Physiol 1959;14:81-3. [Crossref] [PubMed]
- Milic-Emili J, Mead J, Turner JM. Topography of Esophageal Pressure as a Function of Posture in Man. J Appl Physiol 1964;19:212-6. [Crossref] [PubMed]
- Steier J, Jolley CJ, Seymour J, et al. Neural respiratory drive in obesity. Thorax 2009;64:719-25. [Crossref] [PubMed]
- Owens RL, Campana LM, Hess L, et al. Sitting and supine esophageal pressures in overweight and obese subjects. Obesity 2012;20:2354-60. [Crossref] [PubMed]
- Malbrain ML, Cheatham ML, Kirkpatrick A, et al. Results from the International Conference of Experts on Intra-abdominal Hypertension and Abdominal Compartment Syndrome. I. Definitions. Intensive Care Med 2006;32:1722-32.
- Schein M, Ivatury R. Intra-abdominal hypertension and the abdominal compartment syndrome. Br J Surg 1998;85:1027-8. [Crossref] [PubMed]
- Malbrain ML, Chiumello D, Pelosi P, et al. Incidence and prognosis of intraabdominal hypertension in a mixed population of critically ill patients: a multiple-center epidemiological study. Crit Care Med 2005;33:315-22. [Crossref] [PubMed]
- Gurusamy KS, Samraj K, Davidson BR. Low pressure versus standard pressure pneumoperitoneum in laparoscopic cholecystectomy. Cochrane Database Syst Rev 2009;CD006930 [PubMed]
Cite this article as: Lehavi A, Livshits B, Katz Y. Effect of position and pneumoperitoneum on respiratory mechanics and transpulmonary pressure during laparoscopic surgery. Laparosc Surg 2018;2:60.


