Laparoscopic approach to ventral incisional hernia: absorbable or non-absorbable tacks? —a meta-analysis
Introduction
An incisional abdominal hernia is a relative common surgical problem after laparotomies with a not negligible historical incidence and symptomatic cases (1).
Laparoscopic approach for ventral incisional hernia is both a safe and effective strategy to repair abdominal parietal defects, gaining wide acceptance as a valid alternative to classical open approaches (2). Favors for a minimally invasive strategy lie first of all upon patients’ outcomes, such as less surgical site infections, shorter hospital stay and an early return to daily activities (3). However, notwithstanding these evidences and the advent of new strategies from a daily flooded device market, chronic postoperative pain and minor morbidities still argue relevant complaints especially on tack fixation methods (4,5), although these latters are often preferred due to their feasibility and effectiveness (6). Basing on this controversially discussed topic and the effects on both short- and long-term outcome after laparoscopic ventral incisional hernia repair (LVIHR), the safety of absorbable tack (AT) and non-AT (NAT) fixation technique has been investigated through a systematic review and meta-analysis by evaluating their pooled influence on postoperative morbidities.
Methods
Study design
A PubMed-MEDLINE Embase, Google Scholar literature research was carried out by four investigators from the authors’ panel in order to identify relevant articles published from Jan 01, 2013 to Sep 30, 2018. The choice of a defined time interval should be traced back to the attempt of a homogeneous comparison among studies on the basis of a consolidated skill expertise on techniques and the availability of latest generation devices and material resources. The medical subject heading (MeSH) terms at the Boolean function were as follows: ((((((((((laparoscopic) AND incisional hernia) OR ventral hernia) AND repair) AND absorbable) AND non-absorbable) OR titanium) AND tacks) OR tackers) AND ("2013/01/01"[PDAT]: "2018/09/30"[PDAT])). In addition to this process, a manual selection from unidentified references was included, with the last search run on October 10, 2018. All potentially relevant articles were reviewed and checked through a three-phase process (title, abstract and full-text evaluation) basing on the following inclusion criteria: (I) LVIHR; (II) cohort analysis between absorbable and NAT fixation techniques; (III) exhaustive description of surgical techniques; (IV) clearly definition of patients’ outcome according to short-term and long-term morbidities; (V) articles written only in English. Only prospective randomized-controlled trials (RCT) were included, as the poor statistical relevance of the other types of articles (i.e., review, single-center original articles, retrospective articles, states of art and case reports). Trials comparing laparoscopic versus open approaches as far as experimental reports were excluded. All selected articles were individually analyzed with subsequent data extraction by three independent reviewers to collect the following information: authors, year of publication, country of publication, the period of enrollment and number of patients, study inclusion criteria (if applicable) and surgical technique (Table 1).
Table 1
| Author | Year | Country | Type of study | Period | Enrolled patients | Inclusion criteria | Technique |
|---|---|---|---|---|---|---|---|
| Christoffers | 2015 | Denmark | National PSRT | 2008–2012 | 816 | NA | NA |
| Colak | 2015 | Turkey | Single center RCT | 2010–2014 | 51 | Elective surgery | AT Group: AbsorbaTack®, Covidien; NAT Group: Protack®, Tyco Healthcare |
| Bansal | 2016 | India | Single center RCT | 2012–2014 | 90 | Incisional or primary ventral hernia up to 15 cm in size | AT Group: Securestrap®, Ethicon; NAT Group: Protack®, Tyco Healthcare |
| Stirler | 2017 | Netherlands | Single center RCT | 2013–2015 | 80 | Hernia up to 2 cm | AT Group: Securestrap®, Ethicon; NAT Group: Protack ®, Tyco Healthcare |
| Vallabhbhai | 2018 | India | Single center RCT | 2015–2017 | 54 | None reported | NA |
PSRT, perspective randomized trial; RCT, randomized controlled trial; NA, not applicable.
Endpoints
The primary endpoint for this analysis was postoperative morbidity in relation to mesh fixation technique (AT vs. NAT).
Secondary endpoints included the evaluation of:
- Postoperative seroma or parietal fluid collections;
- Small bowel obstructions due to adhesions formation;
- Ventral incisional hernia recurrence;
- Chronic pain.
Statistical analysis
The meta-analysis was conducted with Microsoft Excel 2016 (Microsoft®, Redmond, USA) and with IBM SPSS version 20.0 (IBM®, Segrate MI, Italy). All data have been recorded as absolute numbers (N), percentages (%), mean, standard deviation (SD) with their relative 95% confidence interval (95% CI). Statistical differences or correlations between cohorts were evaluated with paired t-test both for categorical and continuous variables.
For each endpoint, a summarized plot according to positive and negative occurrences was constructed. Odds ratio (OR) was calculated on the basis of the formula: N exposed group with a bad outcome/N exposed group with a good outcome upon N control group with bad outcome/N control group with good outcome. In order to assess the overall test effect for each analyzed endpoint, Z-level function was derived. A value <0.05 was considered statistically significant for both Z and P values.
Moreover, OR forest plots were derived for each article’s item and for cumulative occurrences, according to their weight percentage. In addition, publication bias was evaluated by a funnel plotting asymmetry test with relative standard error (SE), 95% limit (σ2 SD), 99.9% (σ3 SD) limit and a trend line with its relative p-coefficient. A P value less than 0.05 indicated the presence of asymmetry and therefore of selection bias.
Results
Data extraction process
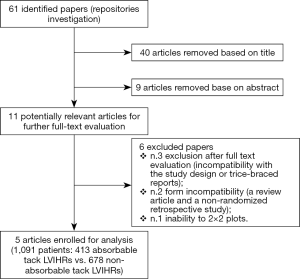
After a primary evaluation according to the Boolean function, 61 relevant articles were identified by four independent investigators for further analysis. Thereafter, 40 were removed on title evaluation and subsequently ulterior nine in accordance with their abstract. Concerning the remaining 11 potentially relevant articles, a second-step analysis was brought throughout a full-text evaluation. Only five articles were enrolled for meta-analysis (7-11) (Table 1). In particular, six papers were excluded due to: (I) incompatibility of the study design or trice-braced cohort studies (three articles); (II) form incompatibility (a review article and a non-randomized retrospective study) and finally, (III) inability to extract patients’ cohorts due to lack of relevant data. At the end of the process, 1,091 patients (413 AT LVIHR and 678 NAT LVIHR) were enrolled (Figure 1).
Quality assessment
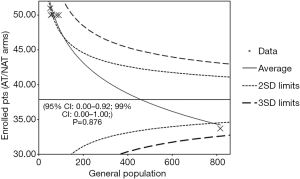
Firstly, a primary search for potential articles’ selection bias was evaluated through an asymmetry funnel plotting test which confirmed statistical heterogeneity among the enrolled population (95% CI: 0.00–0.92; 99% CI: 0.00–1.00; P=0.876) (Figure 2).
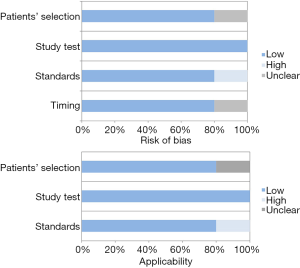
Further quality analysis of the eligible articles was carried out according to QUADAS-2 criteria (http://www.gimbe.org/pagine/1101/it/quadas2), as reported in Table 2. Sources of bias were found in standards and protocols in one study and in the same one, some issues regarding patients’ selection and study timing resulted unclear. Concerning with applicability, patients’ selection was unclear in one study with high risk of bias for standards and protocols (Figure 3).
Table 2
| Author | Risk of bias | Applicability | ||||||
|---|---|---|---|---|---|---|---|---|
| Patients’ selection | Study test | Standards | Timing | Patients’ selection | Study test | Standards | ||
| Christoffers |
L | L | L | L | L | L | L | |
| Colak |
L | L | L | L | L | L | L | |
| Bansal |
L | L | L | L | L | L | L | |
| Stirler |
L | L | L | L | L | L | L | |
| Vallabhbhai |
U | L | H | U | U | L | H | |
L, low; U, unclear; H, high.
Patients’ cohorts evaluation
Accounting 1,091 enrolled patients into two cohorts (413 AT vs. 678 NAT), no significant differences for gender, mean age and defect size were reported (male/female: 174/239 vs. 309/369, 95% CI: −2.64 to 9.44, P=0.267, mean age: 51.67±6.35 vs. 52.11±6.64 years, 95% CI: −0.36 to 1.24, P=0.289 and defect size: 27.29±29.94 vs. 28.95±28.88, 95% CI: −1.93 to 5.25, P=0.364, respectively). However, concerning body mass index (BMI), mean NAT group BMI was significant superior than its counterpart (BMI AT vs. NAT: 28.91±2.84 vs. 29.64±3.96 kg/m2, 95% CI: 0.29–1.17, P=0.001) (Table 3).
Table 3
| Demographics | Enrolled pts (N=1,091) | 95% CI | P value | |
|---|---|---|---|---|
| Absorbable tacks (N=413) | Non-absorbable tacks (N= 678) | |||
| Gender (%) | −2.64 to 9.44 | 0.267 | ||
| Male | 174 (42.13) | 309 (45.57) | ||
| Female | 239 (57.87) | 369 (54.43) | ||
| Age (SD) (years) | 51.67 (6.35) | 52.11 (6.64) | −0.36 to 1.24 | 0.289 |
| BMI (SD) (kg/m2) | 28.91 (2.84) | 29.64 (3.96) | 0.29–1.17 | 0.001 |
| Defect size (SD) (cm2) | 27.29 (29.94) | 28.95 (28.88) | −1.93 to 5.25 | 0.364 |
| N. tacks (SD) | 11.9 (14.00) | 15.47 (18.77) | 1.47–5.67 | 0.001 |
| Operative time (SD) (min) | 100.55 (33.16) | 94.90 (38.32) | −10.11 to 1.18 | 0.013 |
SD, standard deviation; 95% CI, 95% confidence interval.
Surgical data
Notwithstanding comparable surgical approaches, more tacks were fixed in NAT group (AT vs. NAT: 11.90±14.00 vs. 15.47±18.77, 95% CI: 1.47–5.67, P=0.001), though related mean operative time was inferior to AT cohort (AT vs. NAT: 100.55±33.16 vs. 94.90±38.32 min, 95% CI: −10.11 to 1.18, P=0.013) (Table 3).
Short and long-term outcomes
Postoperative morbidity
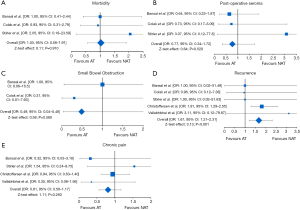
Postoperative complications were reported in three studies, enrolling 211 patients (AT vs. NAT: 111 vs. 110). At the weighted-pooled analysis, no significant cumulative effect was found (40.72% vs. 23.08% vs. 36.20%, P=0.584). With a rough morbidity incidence of 25.22% and 24.54%, there was no difference between cohorts (OR: 1.03, 95% CI: 0.56–1.91, P=0.910) with a cumulative Z-test effect of 0.11 (Table 4) (Figure 4A).
Table 4
| Outcomes | No. patients | AT | NAT | OR | 95% CI | P value | |||
|---|---|---|---|---|---|---|---|---|---|
| N | % (mean) | N | % (mean) | ||||||
| Morbidity | 211 | 111 | 25.22 | 110 | 24.54 | 1.03 | 0.56–1.91 | 0.910 | |
| Hospital stay (days) | 1,091 | 431 | (2.07±0.04) | 678 | (1.89±0.85) | – | −0.26 to 0.09 | <0.001 | |
| Seromas | 211 | 111 | 10.81 | 110 | 13.63 | 0.77 | 0.34–1.72 | 0.520 | |
| Small bowel obstruction | 141 | 71 | 1.41 | 70 | 2.85 | 0.49 | 0.04–5.48 | 0.560 | |
| Recurrence | 1,091 | 431 | 19.61 | 678 | 14.60 | 1.67 | 1.21–2.31 | <0.001 | |
| Chronic pain | 1,041 | 387 | 12.66 | 653 | 15.16 | 0.81 | 0.56–1.17 | 0.260 | |
AT, absorbable tacks; NAT, non-absorbable tacks.
Postoperative hospital stay
Hospital stay was significantly longer in AT group when compared to non-absorbable one (2.07±0.04 vs. 1.89±0.85 days, 95% CI: −0.26 to 0.09, P<0.001) (Table 4).
Postoperative seromas
Postoperative fluid collections were reported in three studies, enrolling 211 patients (AT vs. NAT: 111 vs. 110). At the weighted-pooled analysis, no significant cumulative effect was found (40.72% vs. 23.08% vs. 36.20%, P=0.584). With a rough incidence of 10.81% and 13.63%, there was no difference between cohorts (OR: 0.77, 95% CI: 0.34–1.72, P=0.520) with a cumulative Z-test effect of 0.64 (Table 4) (Figure 4B).
Small bowel obstruction
Postoperative peritoneal adhesions were reported in two studies, enrolling 141 patients (AT vs. NAT: 71 vs. 70). At the weighted-pooled analysis, a significant cumulative effect from one study was reported (63.83% vs. 36.17%, P<0.001). With a rough adhesion incidence of 1.41% and 2.85%, there was no difference between cohorts (OR: 0.49, 95% CI: 0.04–5.48, P=0.560) with a cumulative Z-test effect of 0.58 (Table 4) (Figure 4C).
Recurrence
Recurrences were reported in five studies, enrolling 1,091 patients (AT vs. NAT: 413 vs. 678). At the weighted-pooled analysis, a significant cumulative effect from one study was reported (8.25% vs. 4.67% vs. 7.33% vs. 74.79% vs. 4.94%, P=0.018). With a rough incidence of 19.61% and 14.60%, there was difference between cohorts with a cumulative Z-test effect of 3.13 and favouring NAT fixation technique (Table 4) (Figure 4D).
Chronic pain
Chronic pain was reported in four studies, enrolling 1,040 patients (AT vs. NAT: 387 vs. 653). At the weighted-pooled analysis, a significant cumulative effect from one study was reported (8.65% vs. 7.69% vs. 78.46% vs. 5.19%, P=0.037). With a rough chronic pain (more than the third postoperative month) incidence of 12.66% and 15.16%, there was no difference between cohorts (OR: 0.81, 95% CI: 0.56–1.17, P=0.260) with a cumulative Z-test effect of 1.11 (Table 4) (Figure 4E).
Discussion
An incisional hernia, an abdominal parietal defect, results from a failure of fascial layers healing and its incidence is historically estimated up to 20% of laparotomies with a not negligible percentage of symptomatic cases (12). Among these, almost 90% early develop within three years after initial surgery (13). However, notwithstanding its pathological and socioeconomic impact on patients’ quality of life and loss of productivity, current management still claims debate especially in face of serious complications such as the onset of chronic pain, bowel obstruction or strangulation (14). If minimally invasive surgical strategies should be advised, as stated by the International Endohernia Society guidelines (2), laparoscopic repair is not always suitable, especially for large size groins or for parietal defects close to costal margins or pelvis (15). These techniques include both intraperitoneal and extraperitoneal onlay mesh positioning with or without primary fascial closure and secured with either tacks or sutures and carry many advantages such as low recurrence rates, shorter hospital stay, good cosmetic outcome and low complication rates as compared with open approaches (16).
Recurrence is one of the most important issues of incisional and ventral hernia repair and remains an unsolved clinical issue with increased morbidity, redo surgery rates, longer hospital stay and mortality (17). According to previous reports, recurrence rates range from 2.5% to 9.8% (18-20), while in our analysis incidence reached 16.49% of cases. Several putative contributing factors, such as pathological and technical ones, have been advocated. With regards with the previous ones, mild to severe obesity (BMI >35 kg/m2), smoking status and secondary diastasis recti significantly predispose to relapse (17). On the other hand, an incomplete anterior rectal fascia closure, post-operative infection, mash spillage or shrinkage and inadequate fixation are predisposing factors (18). Although several methods of suturing have been reported, there is no consensus about the optimal strategy (21), though both non-absorbable and AT mesh fixation techniques have been widely accepted.
Concerning with biodegradable devices, they could present the theoretical possibility of loss of tensile strength over time leading to mesh migration, shrinkage or fixation failure due to their biomechanical properties. In this regard, results seem to support these evidence as being AT technique at risk of postoperative relapse (OR: 1.67, 95% CI: 1.21–2.31, P<0.001). In contrast, Lepere et al. (22), in a multicenter study enrolling 105 patients with abdominal parietal defects and surgically treated with resorbable fixation devices, reported no recurrences, but follow-up was limited by embracing only one year. Cavallaro et al. (23), in a non-randomized retrospective study involving 38 incisional hernia patients, reported no difference in recurrence between titanium and AT groups (7.14% vs. 3.85%). However, results seem to be influenced by an asymmetrical distribution of cases, as being M2-M4 (i.e., epigastric and infraumbilical) hernias more common in the absorbable than in the titanium brace (n: 12 vs. 2).
Laparoscopic mesh fixation in regarded particularly painful (24,25). Physiopathologically, helical tacks may cause peritoneal irritation, muscle or vessel injury as far as nerve entrapment (26). For these reasons, non-invasive fixation strategies have been recently proposed on the attempt to optimize post-LIVHR pain, yielding a number of reports over the recent years (27,28). However, publications lack uniformity in outcome description due to several scores used to evaluate preoperative and postoperative pain and thus leading to insufficient recommendations on which approach should be adopted. According to our results, there was no difference in chronic pain between cohorts (AT vs. NAT: 12.66% vs. 15.16%; OR: 0.81, 95% CI: 0.56–1.17, P=0.260), which is consistent with those reported by Reynvoet et al. (6) who, in a systematic review, found no difference in postoperative pain according to technique. In this regard, the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) (29) recommend a case-based approach on fixation technique by considering size, shape and location of the hernia defect. Moreover, neither the defect extension nor the number of tacks influence postoperative pain, as being no cumulative effects between number of fixation points and chronic neuralgia (30).
Schoenmaeckers et al. (31), investigating the effects of tack fixation in a double cohort study enrolling eighty patients, concluded Visual Analogue Scale (VAS) score was so low from a clinical point of view that fewer tacks did not create less pain, nor do more tacks create more pain. Otherwise speculating about some differences about absorbable fixation, Lepere et al. (22) showed at first postoperative month only 10% of patients suffered from low pain (VAS scores: 0.3–3.1) and 98% of them were totally pain-free at 1 year.
Concerning with seromas or postoperative fluid collections, they appear to be a common event after laparoscopic incisional hernia repair which unless a proper diagnosis could lead to detrimental strategies such as reinterventions. We found an incidence of 12.22% in our series, which is consistent with those reported by Sodergren and Switft (32). However, tack adoption does not influence them (OR: 0.77, 95% CI: 0.34–1.72, P=0.52) rather than size of peritoneal sac or a high BMI.
Finally, according to our results, the mean operative time was significantly longer in the AT cohort (100.55±33.16 vs. 94.90±38.32 min, P=0.013), reasons remain unclear. In fact, both types of fixation should be taken relatively the same time intraoperatively. One could argue some differences in penetration power or material properties to achieve fixation which could influence the timing and device feasibility, but data on this aspect still lack and experimental model studies urge. On the other hand, another reason could be found in surgical bias in the adoption of absorbable devices wrongly weaker perceived and leading to the application of more tack or trans-fascial sutures rather than in non-absorbable cases.
Limits of the study
Although a systematic approach, our conclusions should be interpreted in the context of some limitations: first, most of eligible articles had a low sample size with an undeniable possibility of type 2 error; and second, at the weighted-pooled analysis, one study (7) strongly influenced evidence, as reported for recurrences, chronic pain and the risk of small bowel obstructions. On the other hand, notwithstanding these limitations and an explicit approach, overall Z-test effect significance was reached only at relapse analysis with an undeniable level of absolute recommendation (Z=3.13).
Conclusions
The adoption of ATs or NATs for mesh fixation in laparoscopic incisional hernia repair does not influence patients’ clinical outcome and quality of life, except for an increased risk of recurrence when a biodegradable device is used. Therefore, their preference should be dictated by the coexistence of predisposing risk factors for recurrence, such as patients’ comorbidities, and not by presumed technical device properties.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: The authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ls.2018.11.03). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Pollock AV, Evans M. Early prediction of late incisional hernias. Br J Surg 1989;76:953-4. [Crossref] [PubMed]
- Bittner R, Bingener-Casey J, Dietz U, et al. Guidelines for laparoscopic treatment of ventral and incisional abdominal wall hernias (International Endohernia Society (IEHS)-part 1. Surg Endosc 2014;28:2-29. [Crossref] [PubMed]
- Chatzimavroudis G, Kalaitzis S, Voloudakis N, et al. Evaluation of four mesh fixation methods in an experimental model of ventral hernia repair. J Surg Res 2017;212:253-9. [Crossref] [PubMed]
- Misra MC, Bansal VK, Kulkarni MP, et al. Comparison of laparoscopic and open repair of incisional and primary ventral hernia: results of a prospective randomized study. Surg Endosc 2006;20:1839-45. [Crossref] [PubMed]
- Barbaros U, Asoglu O, Seven R, et al. The comparison of laparoscopic and open ventral hernia repairs: a prospective randomized study. Hernia 2007;11:51-6. [Crossref] [PubMed]
- Reynvoet E, Deschepper E, Rogiers X, et al. Laparoscopic ventral hernia repair: is there an optimal mesh fixation technique? A systematic review. Langenbecks Arch Surg 2014;399:55-63. [Crossref] [PubMed]
- Christoffersen MW, Brandt E, Helgstrand F, et al. Recurrence rate after absorbable tack fixation of mesh in laparoscopic incisional hernia repair. Br J Surg 2015;102:541-7. [Crossref] [PubMed]
- Colak E, Ozlem N, Kucuk GO, et al. Prospective randomized trial of mesh fixation with absorbable versus nonabsorbable tacker in laparoscopic ventral incisional hernia repair. Int J Clin Exp Med 2015;8:21611-6. [PubMed]
- Bansal VK, Asuri K, Panaiyadiyan S, et al. Comparison of Absorbable Versus Nonabsorbable Tackers in Terms of Long-term Outcomes, Chronic Pain, and Quality of Life After Laparoscopic Incisional Hernia Repair: A Randomized Study. Surg Laparosc Endosc Percutan Tech 2016;26:476-83. [Crossref] [PubMed]
- Stirler VMA, Nallayici EG, de Haas RJ, et al. Postoperative Pain After Laparoscopic Repair of Primary Umbilical Hernia: Titanium Tacks Versus Absorbable Tacks: A Prospective Comparative Cohort Analysis of 80 Patients With a Long-term Follow-up. Surg Laparosc Endosc Percutan Tech 2017;27:424-7. [Crossref] [PubMed]
- Vallabhbhai DS, Saxena K, Gupta N, et al. A comparative study of mesh fixation by absorbable versus nonabsorbable tacks in laparoscopic ventral hernia repair. Int J Sci Res (Ahmedabad) 2018;7:5-8.
- Le Huu Nho R, Mege D, Ouaïssi M, et al. Incidence and prevention of ventral incisional hernia. J Visc Surg 2012;149:e3-14. [Crossref] [PubMed]
- Ellis H, Gajraj H, George CD. Incisional hernias: when do they occur? Br J Surg 1983;70:290-1. [Crossref] [PubMed]
- Kingsnorth A, Banerjea A, Bhargava A. Incisional hernia repair - laparoscopic or open surgery? Ann R Coll Surg Engl 2009;91:631-6. [Crossref] [PubMed]
- Misiakos EP, Machairas A, Patapis P, et al. Laparoscopic ventral hernia repair: pros and cons compared with open hernia repair. JSLS 2008;12:117-25. [PubMed]
- Kumar D, Khan H, Qureshi MS. Outcome of four years experience in laparoscopic ventral hernia repair. Pak J Med Sci 2015;31:987-90. [PubMed]
- Van Besien J, Vindevoghel K, Sommeling C. Central mesh failure after laparoscopic IPOM procedure. Acta Chir Belg 2016;116:313-5. [Crossref] [PubMed]
- Awad ZT, Puri V, LeBlanc K, et al. Mechanisms of ventral hernia recurrence after mesh repair and a new proposed classification. J Am Coll Surg 2005;201:132-40. [Crossref] [PubMed]
- Nardi M, Millo P, Brachet Contul R, et al. Laparoscopic ventral hernia repair with composite mesh: Analysis of risk factors for recurrence in 185 patients with 5 years follow-up. Int J Surg 2017;40:38-44. [Crossref] [PubMed]
- Mercoli H, Tzedakis S, D’Urso A, et al. Postoperative complications as an independent risk factor for recurrence after laparoscopic ventral hernia repair: a prospective study of 417 patients with long-term follow-up. Surg Endosc 2017;31:1469-77. [Crossref] [PubMed]
- Sadava EE, Krpata DM, Gao Y, et al. Laparoscopic mechanical fixation devices: does firing angle matter? Surg Endosc 2013;27:2076-81. [Crossref] [PubMed]
- Lepere M, Benchetrit S, Bertrand JC, et al. Laparoscopic resorbable mesh fixation. Assessment of an innovative disposable instrument delivering resorbable fixation devices: I-Clip(TM). Final results of a prospective multicentre clinical trial. Hernia 2008;12:177-83. [Crossref] [PubMed]
- Cavallaro G, Campanile FC, Rizzello M, et al. Lightweight polypropylene mesh fixation in laparoscopic incisional hernia repair. Minim Invasive Ther Allied Technol 2013;22:283-7. [Crossref] [PubMed]
- Eid GM, Prince JM, Mattar SG, et al. Medium-term follow-up confirms the safety and durability of laparoscopic ventral hernia repair with PTFE. Surgery 2003;134:599-603; discussion 603-4. [Crossref] [PubMed]
- Berger D, Bientzle M, Müller A. Postoperative complications after laparoscopic incisional hernia repair. Incidence and treatment. Surg Endosc 2002;16:1720-3. [Crossref] [PubMed]
- Nguyen SQ, Divino CM, Buch KE, et al. Postoperative pain after laparoscopic ventral hernia repair: a prospective comparison of sutures versus tacks. JSLS 2008;12:113-6. [PubMed]
- Eriksen JR, Bech JI, Linnemann D, et al. Laparoscopic intraperitoneal mesh fixation with fibrin sealant (Tisseel) vs. titanium tacks: a randomised controlled experimental study in pigs. Hernia 2008;12:483-91. [Crossref] [PubMed]
- Olmi S, Scaini A, Erba L, et al. Use of fibrin glue (Tissucol) in laparoscopic repair of abdominal wall defects: preliminary experience. Surg Endosc 2007;21:409-13. [Crossref] [PubMed]
- Earle D, Roth JS, Saber A, et al. SAGES guidelines for laparoscopic ventral hernia repair. Surg Endosc 2016;30:3163-83. [Crossref] [PubMed]
- Wassenaar E, Schoenmaeckers E, Raymakers J, et al. Mesh-fixation method and pain and quality of life after laparoscopic ventral or incisional hernia repair: a randomized trial of three fixation techniques. Surg Endosc 2010;24:1296-302. [Crossref] [PubMed]
- Schoenmaeckers EJP, de Haas RJ, Stirler V, et al. Impact of the number of tacks on postoperative pain in laparoscopic repair of ventral hernias: do more tacks cause more pain? Surg Endosc 2012;26:357-60. [Crossref] [PubMed]
- Sodergren MH, Swift I. Seroma Formation and Method of Mesh Fixation in Laparoscopic Ventral Hernia Repair — Highlights of a Case SERIES. Scand J Surg 2010;99:24-7. [Crossref] [PubMed]
Cite this article as: Barone M, Raimondi P, Caldaralo F, Cichella A, Tannous M, Ciampaglia F, Cipollone G, Cotellese R, Mucilli F, Innocenti P, Di Bartolomeo N. Laparoscopic approach to ventral incisional hernia: absorbable or non-absorbable tacks? —a meta-analysis. Laparosc Surg 2018;2:63.