Laparoscopic umbilical herniorrhaphy: a novel technique of hernia neck closure and outcomes in the first 19 cases
Introduction
An abdominal wall hernia is the abnormal protrusion of abdominal contents, primarily fatty tissue, omentum or small bowel, through a defect in the abdominal musculature (1). Hernias are classified by location or may be classified as acquired or congenital. They are a common surgical problem with approximately 800,000 inguinal herniorrhaphies being performed in the United States each year (2). In 2011, Dabbas et al. reported the modern relative frequency of herniorrhaphy as: inguinal, umbilical, epigastric, incisional, periumbilical, femoral and other rare types such as a Spighelian hernia (3).
While watchful waiting is an option in the management of umbilical hernias, an elective repair is usually offered to patients who are good surgical candidates (4). Elective repair for all symptomatic hernias should be performed due to the risk of incarceration, bowel obstruction, and strangulation and their association with a higher morbidity (5).
Inguinal and umbilical hernias, in retrospective studies, are at the highest risk for strangulation and emergency surgery (6). Asymptomatic umbilical hernias less than 2 centimeters in diameter can reasonably be managed with careful monitoring and follow up. Strosberg et al. in 2017 reported that patients without an umbilical hernia repair had more days in hospital and more time off work than a matched cohort with a laparoscopic repair and suggested that despite the cost of surgery the impact on community economics is greater for those who do not have a surgical repair (7).
The repair of inguinal hernias is standardized across the surgical community thanks to the robust evidence of laparoscopic mesh repairs. Umbilical herniorrhaphy is more diverse in approach and open repairs are commonly performed. A few studies have consistently reported that laparoscopic repair is associated with a shortened time in hospital and better control of pain in the post-operative period (8-10). Studies have also shown improved rates of wound infection, hernia recurrence, and wound dehiscence.
The traditional laparoscopic repair of an umbilical hernia involves standard insufflation of the intra peritoneal abdominal cavity and placement of laparoscopic ports. The herniated tissue is reduced into the abdominal cavity and a synthetic underlay mesh is placed over the abdominal wall defect usually with a 2 cm overlap and secured in place with tacks or sutures. Our approach has been to repair the hernia neck laparoscopically with intracorporeal sutures before placing an underlay mesh, resulting in better cosmesis and lower risk of recurrence than a traditional laparoscopic mesh repair.
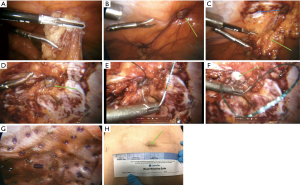
A similar approach by Costa et al. (11) in 2016 involved a minimally invasive technique with 3 laparoscopic ports. Adhesiolysis is performed and the midline from 4 cm below the umbilicus to the epigastric region, is closed with a laparoscopic stapler. A mesh is then placed in the retrorectus space and secured with absorbable tacks. A single surgeon in a regional hospital has developed a similar technique (Figure 1). It involves closing the neck of the hernia to re-establish normal abdominal wall anatomy with laparoscopic suturing rather than staples. A preperitoneal mesh is then placed and secured with absorbable tacks.
The theoretical benefits of closing the umbilical hernia neck with sutures include better cosmesis and a lower risk of recurrence. Closure of the hernia neck reduces the operating time and limits the risk of infection when compared to closing the entire midline as in Costa’s technique (11). A minimally invasive approach also improves post-op pain scores, limits hospital admission, and allows surgeons to identify other intra-abdominal pathology such as additional hernias which may be simultaneously repaired.
Methods
At a regional hospital in northern Saskatchewan, Canada an individual surgeon has performed 19 umbilical and periumbilical hernia repairs with a novel new technique. In this technique the surgeon insufflates the peritoneal cavity and places three laparoscopic ports (Figure 2).

Initially the abdominal wall is inspected to identify other pathology such as concomitant hernias. The umbilical or para umbilical hernia is then reduced and adhesions are released (Figure 1A).
The hernia neck is identified (Figure 1B,C) and an overlap of 2 cm is marked out on the abdominal wall in all four directions (Figure 1D). This is later used when applying the underlay mesh.
The fascial defect is then closed laparoscopically with a suture to restore the abdominal wall anatomy. A V-loc© non absorbable suture is used (Figure 1E). A synthetic dual layer Ventralite© mesh is then placed over the sutured hernia neck and secured with absorbable hernia tacks (Figure 1G). Care is taken to ensure a 2 cm overlap of the hernia neck based on the abdominal wall markings. Patients were discharged as soon as they felt well enough to go home (Figure 3).

The formal operating room reports, the surgeon’s dictated surgery reports and the preoperative patient evaluation were used to identify the length of surgery, hospital stay, body mass index (BMI) and demographics for each patient.
Ethics approval was not obtained for the study as we did not involve the patients directly in the study. Informed consent was obtained from all 19 patients for video recording and picture taking as required prior to the surgery and as part of the informed consent process.
Results
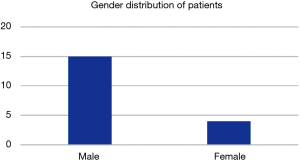
Nineteen cases were evaluated in patients aged 34–67, the majority of whom were male (88%) (Figure 4).
Only one intraoperative complication occurred with an iatrogenic skin rupture at the hernia site. The skin was sutured and the patient made a complete recovery. No further complications such as bowel injury or bleeding were reported.
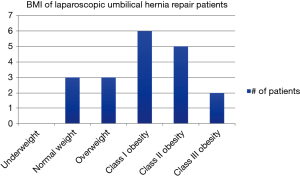
The population was diverse with BMI’s varying from 22.6–45.3 and included those with multiple comorbidities (Figure 5).
With obesity established as a risk factor for recurrent herniation, local practice patterns vary in terms of the BMI that surgeons will consider for an elective repair (13). The surgeon did not select for this procedure based on BMI but rather used it for all candidates who were healthy enough to tolerate a laparoscopic procedure. We believe that this distribution of patient BMI, although small is representative of the general surgical population in our region.
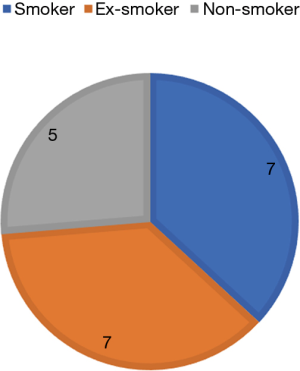
Patients were regularly counselled to quit smoking before their hernia repair as smoking is a well-established risk factor but 7 patients were actively smoking at the time of repair (Figure 6) (14). The smoking did not impact their short-term outcomes, and all 7 made uneventful recoveries.
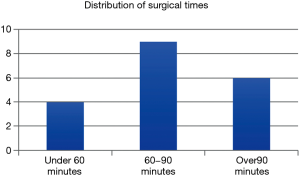
A common concern about the laparoscopic approach is the longer operative time (Figure 7). The average surgical time for laparoscopic umbilical herniorrhaphy was 84.75 minutes including all cases and 74.23 minutes when three cases, each with surgical times of 174, 136 and 123 minutes respectively were excluded from the data. The three excluded cases involved adhesiolysis secondary to a choanal atresia multistep repair as well as the concomitant repair of 2 additional hernias, the removal of an old mesh and the concomitant laparoscopic repair of bilateral inguinal hernias.
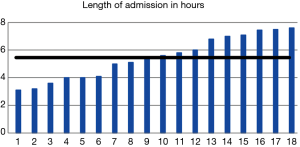
An advantage of laparoscopic surgery over the traditional open approach is the shorter length of hospital admission (Figure 8). The length of stay varied from 3 hours and 7 minutes to one outlier at 14 hours and 35 minutes who experienced significant post-operative nausea. The average stay when the outlier is excluded was 5 hours and 28 minutes. All surgeries were performed as day cases and no patients including the nausea patient, were admitted to our hospital.
Many of the surgeries were video recorded with the informed consent of patients and used for teaching purposes.
Discussion
Laparoscopic umbilical herniorrhaphy with intra corporeal suturing of the hernia neck to restore the abdominal wall anatomy is a valid option for the repair of umbilical and paraumbilical hernias. While the sample size of this study is small, it clearly demonstrates the feasibility of this approach.
These cases will need to be followed up in 2–3 years to evaluate for complications related to the surgical technique. Short term recurrences are thought to be related to surgical technique (15).
To date we have had no hernia recurrences over the past 2 years. There has been no wound infection or seromas either.
This technique has allowed for a relatively quick repair of umbilical hernias with a short length of stay. It is a reasonable approach for those with a greater BMI where increased subcutaneous fatty tissue can make an open repair technically very difficult. The laparoscopic repair with closure of the hernia neck restores the anatomy to normal while producing good cosmesis for the patient and offering an enhanced recovery (Figure 1H).
We extrapolated this data from the component separation technique which restored the rectus abdominis muscle function in the midline resulting in more efficient physiological outcomes (16). This in turn has resulted in decreased recurrence rates with the component separation technique and it is our belief that closure of the umbilical hernia neck will result in similarly reduced recurrence rates, especially in the obese patient cohort.
The incorporation of the skin into the closure of the hernia neck also allows for reconstruction of the umbilicus with good cosmesis especially in female patients who indicated their satisfaction with the outcome (Figure 1F,H).
The greatest advantage so far has been the lack of umbilical wound infections due to the absence of an incision at the umbilicus. This is often an issue in our morbidly obese patients where the subcutaneous tissues can be as deep as 10 cm between the skin and rectus muscle fascia.
By placing our ports in the left upper quadrant and left flank we have avoided potential wound infections at the umbilicus which, while low in most patients is higher in the morbidly obese patient cohort (Figure 2). Colon et al. reported a wound infection rate of 26% in obese patients vs. 4% in patients with a normal BMI who underwent open umbilical herniorrhaphy (17).
A controversial issue has been the use of local anaesthetic in the subcutaneous tissues for obese patients as well as their poor pain control as reported by Kulacoglu et al. (18). Both of these issues have been obviated with the laparoscopic repair and hernia neck suturing in our study. None of our patients had local infiltration into the umbilicus for pain control. There were no post-operative periumbilical pain issues in our patient cohort.
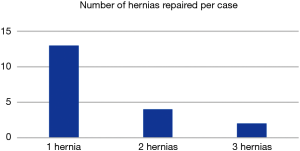
Six of the 19 (32%) patients had more than one hernia present periumbilically (Figure 9). This is another advantage of this technique as in the open repair, additional hernias may have been missed. In 3 of the 6 patients, the additional hernias were not in the midline, which would have made an open repair difficult. Complete laparoscopic visualization of the anterior abdominal wall allows us to visualize the additional hernias and affect a repair.
This is a pilot project involving the first 19 patients and we hope in time to expand the study to involve more surgeons and patients. We will also need to look at the long term complication rates of this repair as well as we currently only have a two year follow up.
The use of the V-loc© suture did not present any issues as it was covered by the dual layer Ventralite mesh© (Figure 1G). The Ventralite© mesh is a dual layer mesh with one side consisting of an absorbable hydrogel barrier facing the bowel which reduces the risk of bowel adhesions.
The side facing the abdominal wall is non-absorbable prolene and is responsible for fibrosis.
One of the disadvantages of this study has been the steep learning curve involved in the laparoscopic intracorporeal suturing of the hernia neck with non-absorbable suture. This has resulted in operating times of more than 60 minutes in the majority of patients (Figure 7). We feel this will be reduced with greater surgical experience once the learning curve has been breached and significant muscle memory retained. Given that the average open umbilical repair often takes less than 30 minutes to perform, this may be a contentious issue until proficiency with this technique is obtained. Four cases have been performed under 60 minutes and we hope to continue this trend with future repairs (Figure 7).
Conclusions
Laparoscopic umbilical herniorrhaphy with intra corporeal suturing of the hernia neck is a novel technique to tackle an old issue. We hope that with greater surgeon experience, operative times will improve leading to the economic feasibility of this approach. As minimally invasive techniques continue to become the standard of care and surgical training focuses more on laparoscopic techniques, this approach may become a valuable addition to the surgical armamentarium for paraumbilical and umbilical hernia repairs especially in the obese patient cohort.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ls.2018.11.08). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Ethics approval was not obtained for the study as we did not involve the patients directly in the study. Informed consent was obtained from all 19 patients for video recording and picture taking as required prior to the surgery and as part of the informed consent process.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Hernias of the Abdominal Wall. Available online: https://www.merckmanuals.com/en-ca/professional/gastrointestinal-disorders/acute-abdomen-and-surgical-gastroenterology/hernias-of-the-abdominal-wall. Accessed November 18, 2017.
- Rutkow IM. Demographic and socioeconomic aspects of hernia repair in the United States in 2003. Surg Clin North Am 2003;83:1045-51. v-vi. [Crossref] [PubMed]
- Dabbas N, Adams K, Pearson K. Frequency of abdominal wall hernias: is classical teaching out of date?. JRSM Short Rep 2011;2:5. [Crossref] [PubMed]
- Kokotovic D, Sjølander H, Gögenur I. Watchful waiting as a treatment strategy for patients with a ventral hernia appears to be safe. Hernia 2016;20:281-7. [Crossref] [PubMed]
- Primatesta P, Goldacre MJ. Inguinal hernia repair: incidence of elective and emergency surgery, readmission and mortality. Int J Epidemiol 1996;25:835-9. [Crossref] [PubMed]
- Davies M, Davies C, Morris-Stiff G. Emergency presentation of abdominal hernias: outcome and reasons for delay in treatment - a prospective study. Ann R Coll Surg Engl 2007;89:47-50. [Crossref] [PubMed]
- Strosberg DS, Pittman M, Mikami D. Umbilical hernias: the cost of waiting. Surg Endosc 2017;31:901-6. [Crossref] [PubMed]
- Hajibandeh S, Hajibandeh S, Sreh A. Laparoscopic versus open umbilical or paraumbilical hernia repair: a systematic review and meta-analysis. Hernia 2017;21:905-16. [Crossref] [PubMed]
- Korukonda S, Amaranathan A, Ramakrishnaiah VPN. Laparoscopic versus Open Repair of Para-Umbilical Hernia- A Prospective Comparative Study of Short Term Outcomes. J Clin Diagn Res 2017;11:PC22-PC24. [PubMed]
- Bell-Allen N, O'Rourke H, Hong L. Laparoscopic ventral hernia repair using only 5-mm ports. ANZ J Surg 2017; [Epub ahead of print]. [PubMed]
- Costa TN, Abdalla RZ, Santo MA. Transabdominal midline reconstruction by minimally invasive surgery: technique and results. Hernia 2016;20:257-65. [Crossref] [PubMed]
- Vetter C, Pillay Y. Video showing the steps involved. Asvide 2018;5:908. Available online: http://www.asvide.com/article/view/28811
- Shankar DA, Itani KMF, O'Brien WJ. Factors Associated With Long-term Outcomes of Umbilical Hernia Repair. JAMA Surg 2017;152:461-6. [Crossref] [PubMed]
- Sorensen LT, Friis E, Jorgensen T, et al. Smoking is a risk factor for recurrence of groin hernia. World J Surg 2002;26:397-400. [Crossref] [PubMed]
- Kim LT. Complexity of the "Simple" Umbilical Hernia Repair. JAMA Surg 2017;152:466. [Crossref] [PubMed]
- Butler CE, Baumann DP, Janis JE. Abdominal wall reconstruction. Curr Probl Surg 2013;50:557-86. [Crossref] [PubMed]
- Colon MJ, Kitamura R, Telem DA. Laparoscopic umbilical hernia repair is the preferred approach in obese patients. Am J Surg 2013;205:231-6. [Crossref] [PubMed]
- Kulacoglu H, Yazicioglu D, Ozyaylali I. Prosthetic repair of umbilical hernias in adults with local anesthesia in a day-case setting: a comprehensive report from a specialized hernia center. Hernia 2012;16:163-70. [Crossref] [PubMed]
Cite this article as: Vetter C, Pillay Y. Laparoscopic umbilical herniorrhaphy: a novel technique of hernia neck closure and outcomes in the first 19 cases. Laparosc Surg 2018;2:69.