Case report: laparoscopic-assisted small bowel resection for retained capsule endoscopy using fluoroscopy
Introduction
Capsule endoscopy is a frequently used method to evaluate the small bowel, especially in patients with chronic anemia after the upper and lower endoscopies are non-diagnostic (1). Capsule retention is defined as >2 weeks without passing the capsule and the retention rate is reported in the literature around 1–3% (2). For retained capsules, they can still pass spontaneously if allowed more time but occasionally require retrieval with either push enteroscopy or surgery. A laparoscopic small bowel resection with fluoroscopy should be considered early in the workup of retention as it is both diagnostic and therapeutic. We will describe a case report, brief literature review, and some pearls and pitfalls for retained capsule endoscopy using a laparoscopic fluoroscopy-guided small bowel resection.
Case presentation
This is a 71-year-old female with a history of hypertension, chronic anemia requiring multiple prior blood transfusions, former smoker, and past surgical history of laparoscopic cholecystectomy and total abdominal hysterectomy. She had an extensive workup for her anemia including an upper and lower endoscopy which were non-diagnostic as well as a capsule endoscopy that was placed in September 2017. She failed to pass the capsule and was then sent to a tertiary center for upper push enteroscopy which was unsuccessful at retrieving the device. At that time, the endoscopist injected dye at the most distal aspect of their push enteroscopy to help with future identification. She had multiple abdominal X-rays and CT scans showing the capsule located in the mid-to-distal small bowel in the right side of the abdomen. She never had any obstructive symptoms and was able to tolerate a regular diet without difficulty. The patient was anxious to have the capsule removed as it was causing her stress and anxiety. She was consented for laparoscopic assisted small bowel resection with fluoroscopy, removal of foreign body, possible open procedure, possible ileocecectomy. Her surgery was performed on February 2019.
Patient selection and workup
Our patient selection was dependent on the fact that there was a retained foreign body with a likely underlying etiology that had not been diagnosed.
Pre-operative preparation
We do not use a bowel preparation for small bowel resections since any stool burden should not impact the bowel resection or the procedure. The patient had pre-op labs to monitor for worsening anemia that would require pre-op transfusions. She was typed & screened for blood products.
Equipment preference card
A general diagnostic laparoscopy set-up case card was used.
Procedure
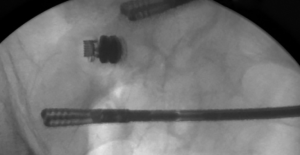
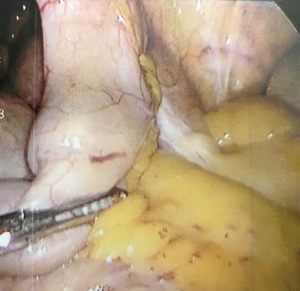
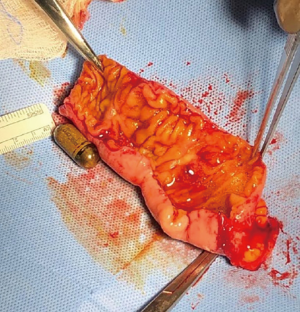
The patient was positioned supine with both arms extended. A 5 mm Optiview trocar was used with a 0° scope under direct vision and pneumoperitoneum was established. Two additional 5 mm ports were placed in the left side of the abdomen. Once the area of concern was identified, the bowel was clamped proximally and distally, and fluoroscopy was used to manipulate the bowel and confirm the segment of bowel contained the capsule (Figure 1). A 5 cm Pfannenstiel incision was then made and that segment of small bowel was exteriorized without removing the graspers (Figure 2). A stapled technique was then used to resect approximately 20 cm of mid ileum. A side-to-side functional end-to-end anastomosis was performed using a 80 mm linear GIA stapler and then primarily closing the common enterotomy channel. Her operation proceeded without any complications and her final pathology returned as non-malignant inflamed segment of bowel with ulcerations suggestive of indolent Crohn’s disease and chronic injury pattern (Figure 3).
Role of team members
The attending surgeon and the senior general surgery resident performed the case with the assistance of a radiology technician for the fluoroscopy portion.
Postoperative management
Patients can be started on a clear liquid diet immediately post-operatively and advanced as tolerated. We use multi-modal pain medications including scheduled Tylenol, Toradol, Gabapentin, and as needed narcotics. We also encourage ambulation and the use of incentive spirometry. The benefit of a laparoscopic assisted approach is a quicker return of bowel function. In addition, we check labs on post-op day #1 to monitor for kidney function and hemoglobin levels. For this patient, given her late onset of symptoms and lack of additional inflammatory symptoms, she did not require any further Crohn’s treatment. She did have a post-op course complicated by acute-blood loss anemia requiring a transfusion of two units of blood, acute kidney injury that was treated with IV fluids and post-operative ileus that resolved spontaneously. She was discharged from the hospital and seen in clinic two weeks post-op and was doing very well without any further complications.
Literature review
Retained capsule endoscopy is described as a capsule that does not pass for >2 weeks and has a reported incidence rate of 1–3%. Retention is usually associated with an underlying malignancy or inflammatory condition (2). Patients with Crohn’s disease have a reported retention rate up to 2.6% (3). In one study of 904 patients undergoing capsule endoscopy, there was a retention rate of 0.88% and a reported 100% success with double balloon push enteroscopy for retrieval of retained capsules but success is dependent on the clinician’s expertise. 62.5% of these patients still elected for surgery to remove the underlying etiology of their retention even after endoscopic removal (4). In a retrospective European study that was performed between 2005–2013 with 359 patients, they had a retention rate of 3.1%. Of these patients, 45.5% was due to ulceration or inflammation, 18.2% malignancy, and 36.4% dysmotility (retained in the esophagus or stomach). For these patients, 45% eventually passed the capsule either spontaneously or with medical therapy (i.e., treating underlying Crohn’s disease), 18% required retrieval with endoscopy and 36% subsequently required surgery. Of those patients that required surgery, the surgery was both diagnostic and therapeutic.
Tips, tricks & pitfalls
A major pitfall of this surgery is missing the primary etiology. It is possible for the capsule to move proximally during the manipulation of the bowel since it acts as a ball-valve. In addition, once you have the segment localized, it is still possible to let go of that segment of bowel prior to resection and then miss the primary etiology. This would then lead to an inaccurate diagnosis by potentially resecting normal non-diseased bowel and thus leaving diseased bowel behind. Ongoing obstructive or inflammatory symptoms would thus prompt a reoperation. The trick to keep this from happening would be to use the fluoroscopy from the very beginning of the operation before manipulating any of the bowel segments and to not remove the graspers until the bowel is exteriorized and resected.
Discussion
Retained capsule endoscopy is rare but highly associated with an underlying etiology of malignancy, stricture, or chronic inflammation. This has traditionally been treated with endoscopy as a first line treatment which adheres to the principle of starting with least invasive to more invasive procedures. Retention of the capsule can ultimately prompt surgical resection and thus lead to a definitive diagnosis. Laparoscopy combined with fluoroscopy can help localize the capsule and minimize the risk of missing the underlying lesion. These lesions typically produce ball-valve mechanisms without complete obstructions and thus it is important to not disrupt the anatomy. We suggest that the laparoscopic assisted approach offers the ability to keep the surgery minimally invasive but avoid inadvertently missing the underlying etiology. Bowel resection should be performed in patients with suspected pathologic reasons for the retention, especially in cases with a very long course of retention as this portion of small bowel will likely cause future partial or complete small bowel obstructions.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ls.2019.09.01). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Declaration of Helsinki (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Ormeci AC, Akyuz F, Baran B, et al. Retention during capsule endoscopy: Is it a real problem in routine practice? J Int Med Res 2016;44:968-75. [Crossref] [PubMed]
- Liao Z, Gao R, Xu C, et al. Indications and detection, completion, and retention rates of small bowel capsule endoscopy: a systematic review. Gastrointest Endosc 2010;71:280-6. [Crossref] [PubMed]
- Xin L, Liao Z, Du YQ, et al. Retained capsule endoscopy causing intestinal obstruction-Endoscopic retrieval by retrograde single-balloon enteroscopy. J Interv Gastroenterol 2012;2:15-8. [Crossref] [PubMed]
- Van Weyenberg SJ, Van Turenhout ST, Bouma G, et al. Double-balloon endoscopy as the primary method for small-bowel video capsule endoscopy retrieval. Gastrointest Endosc 2010;71:535-41. [Crossref] [PubMed]
Cite this article as: Jensen A, Nagamoto T. Case report: laparoscopic-assisted small bowel resection for retained capsule endoscopy using fluoroscopy. Laparosc Surg 2019;3:45.