Hydatid cyst of Morgagni—the case of a misidentified paratubal cyst as an appendiceal mucocele
Introduction
Mucinous tumors of the appendix and ovary/fallopian tubes can have similar presentations. Most commonly, these tumors are asymptomatic and found incidentally during surgery. When symptomatic, these pathologies can present with lower abdominal pain, a palpable abdominal mass, nausea/vomiting, fevers, or leukocytosis. It is uncommon for these tumors to be confused with one another with the increased use and sensitivity of preoperative imaging modalities.
Case presentation
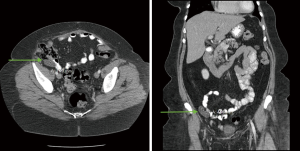
This is the case of a 60-year-old female with a history of hypertension, hyperlipidemia, gastric reflux, and hysterectomy who initially presented to the surgery clinic for evaluation of a ventral hernia. A CT abdomen/pelvis (Figure 1) was obtained which demonstrated an incidental finding: a tubular distended appendix with a pencil thin wall measuring up to 4.5 cm in length and 1.7 cm in width, suggestive of an appendiceal mucocele.
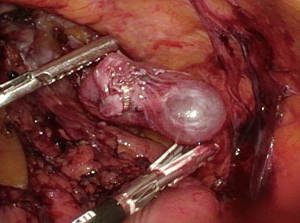
With this finding, the patient was booked for a diagnostic laparoscopy and resection of mucocele. In the operating room, the cecum was mobilized from the lateral abdominal wall and an elongated appendix was identified. The appendix was removed in the usual fashion. Thereafter, a mucinous structure was identified in the right lower quadrant which was adherent to the lateral abdominal wall (Figures 2,3). It was believed to be related to the ovary, so an intraoperative gynecology consult was obtained. It was discussed that most likely the mucinous mass was an ovarian cyst, and the decision was made to remove the suspicious mass using an endobag.
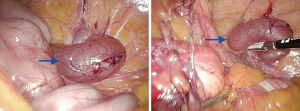
Postoperative pathology confirmed the following: appendix with mild active mucosal inflammation and no evidence of neoplasm, and benign serous cyst lined by tubal epithelium and smooth muscle consistent with paratubal cyst (PTC) (Hydatid Cyst of Morgagni).
Discussion
Appendiceal mucocele was first described in 1,842 by Rokitansky (1,2). It is an obstructive disease process where dilation of the appendix is caused by intraluminal accumulation of mucus, and may be related to either a benign or malignant disease process. There are four different histologic types including retention cyst, mucosal hyperplasia, mucinous cystadenoma, and mucinous cystadenocarcinoma (1,3).
Mucocele of the appendix is a rare disease which is seen in 0.2% to 0.7% of appendectomied specimens. Often times patients are completely asymptomatic (1,3). If symptoms are present, they are generally non-specific and include right lower quadrant abdominal pain, a palpable abdominal mass, nausea/vomiting, or gastrointestinal bleeding. As a result, it is often mistaken for acute appendicitis. Approximately 50% of the time, appendiceal mucocele is discovered accidentally either radiographically or during surgery (1,3,4).
CT imaging is the most accurate diagnostic tool that helps identify mucoceles. CT signs include a well-encapsulated cystic mass, 2 to 20 cm, with potential curvilinear mural wall calcifications (1,3,5). Mucoceles less than 2 cm are usually benign (3). Those measuring 2 cm or greater should be excised to eliminate any potential progression to malignancy (4). CT signs specific to appendiceal mucocele are related to maximal appendix luminal diameter. In a study conducted by Bennett et al., they found that luminal diameter greater than 1.3 cm had 71.4% sensitivity and 94.6% specificity in diagnosing a mucocele of the appendix (5).
It is important to correctly diagnosis appendiceal mucocele prior to surgery, in order to avoid any intraoperative or postoperative complications (1). If Intraoperative spillage occurs, epithelial cells may spread throughout the peritoneal cavity and lead to pseudomyxoma peritonei, which has a high mortality (1,3).
Once the diagnosis has been made of appendiceal mucocele, there still remains debate as to the best surgical approach: open versus laparoscopic. Although no consensus has been made, a specific treatment algorithm was proposed by Dhage-Ivatury and Sugarbaker to help guide therapeutic decisions. Open laparotomy has historically been favored; however, laparoscopy can be safely utilized if the surgeon avoids grasping the mucocele and uses an endo-bag to remove the specimen (1,3).
Mucinous tumors of the appendix and ovary/fallopian tubes are known to occur together. The exact relationship between the two sites remains unclear. However, in association with pseudomyxoma peritonei, it is likely related to metastasis (6,7). Although they may have similar presenting symptoms, it is uncommon for these tumors to be confused with one another due to advances in modern day imaging modalities.
PTCs account for 3–10% of adnexal masses, and are found in the broad ligament between the ovary and fallopian tube (8). PTCs are usually benign, asymptomatic simple cysts, and are incidentally found (8). Symptoms can occur if they rapidly grow, hemorrhage, rupture, or torsion. In these instances, they may share common clinical presentations with diseases such as appendicitis, ruptured ovarian cyst, acute ureteric colic, or pelvic inflammatory disease (8).
A specific subtype of PTC is the hydatid cyst of Morgangi. This refers to a pedunculated or sessile PTC located near the fimbria of the fallopian tube (8,9). Similar to all PTCs, hydatid cysts of Morgangi are frequently asymptomatic and incidental found during laparoscopy (9,10).
Recently, particular attention has been turned towards these cysts, as they have been found to be a cause of unexplained infertility (9,10). Interestingly, a study conducted by Rasheed and Abdelmonem found that removal of hydatid cysts of Morgangi in patients with unexplained infertility lead to a higher rate of spontaneous pregnancy (9).
In general, there is no well-defined criteria for surgical management of PTCs, and they are usually treated the same as any ovarian mass (8). A small, unilocular, simple cyst may be clinically followed over time. A large, persistent, thick walled cyst, with papillary projections, or showing signs of torsion, should be managed surgically (8). Surgery can be performed either laparoscopically or open, depending on the size of the cyst. If performed laparoscopically, basic microsurgical principles should be followed, and bipolar diathermy should be utilized for extraction of the cyst (11).
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: The authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ls.2019.09.03). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Declaration of Helsinki (as revised in 2013). Written informed consent was obtained from the patient for publication of this Case Report and any accompanying images. A copy of the written consent is available for review by the Editors In Chief of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Demetrashvili Z, Chkhaidze M, Khutsishvili K, et al. Mucocele of the appendix: case report and review of literature. Int Surg 2012;97:266-9. [Crossref] [PubMed]
- Abreu Filho JGD, Lira EFD. Mucocele of the appendix: appendectomy or colectomy? J Coloproctol (Rio J) 2011;31:276-84. [Crossref]
- Dhage-Ivatury S, Sugarbaker PH. Update on the surgical approach to mucocele of the appendix. J Am Coll Surg 2006;202:680-4. [Crossref] [PubMed]
- Stocchi L, Wolff BG, Larson DR, et al. Surgical treatment of appendiceal mucocele. Arch Surg 2003;138:585-9; discussion 589-90. [Crossref] [PubMed]
- Bennett GL, Tanpitukpongse TP, Macari M, et al. CT diagnosis of mucocele of the appendix in patients with acute appendicitis. AJR Am J Roentgenol 2009;192:W103-10 [Crossref] [PubMed]
- Seidman JD, Elsayed AM, Sobin LH, et al. Association of mucinous tumors of the ovary and appendix. A clinicopathologic study of 25 cases. Am J Surg Pathol 1993;17:22-34. [Crossref] [PubMed]
- Sumithran E, Susil BJ. Concomitant mucinous tumors of appendix and ovary. Result of a neoplastic field change? Cancer 1992;70:2980-3. [Crossref] [PubMed]
- Kiseli M, Caglar GS, Cengiz SD, et al. Clinical diagnosis and complications of paratubal cysts: review of the literature and report of uncommon presentations. Arch Gynecol Obstet 2012;285:1563-9. [Crossref] [PubMed]
- Rasheed SM, Abdelmonem AM. Hydatid of Morgagni: a possible underestimated cause of unexplained infertility. Eur J Obstet Gynecol Reprod Biol 2011;158:62-6. [Crossref] [PubMed]
- Abd-el-Maeboud KH. Hydatid cyst of Morgagni: any impact on fertility? J Obstet Gynaecol Res 1997;23:427-31. [Crossref] [PubMed]
- Darwish AM, Amin AF, Mohammad SA. Laparoscopic management of paratubal and paraovarian cysts. JSLS 2003;7:101-6. [PubMed]
Cite this article as: Lelchuk A, Nicoara M, Nazir S, Liu S, Bain K. Hydatid cyst of Morgagni—the case of a misidentified paratubal cyst as an appendiceal mucocele. Laparosc Surg 2019;3:46.