A crossover study on the advantage of an additional rotation function in a needle holder compared to a conventional needle holder in a pelvitrainer model
Introduction
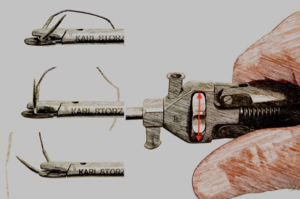
Laparoscopic surgery is an increasingly favoured technique among surgeons. In addition to its cosmetic benefits, it is associated with reduced postoperative infection rates, shorter hospitalization periods, and minimal loss of blood, compared to open surgery (1-3). However, laparoscopic surgery is generally longer in duration, and the operating surgeons tire more rapidly (3,4). Robotic-assisted laparoscopy offers the potential to mitigate these drawbacks, by improving the instruments’ range of motion and ergonomic qualities (5,6). In general, the learning curve of conventional laparoscopic surgery is relatively flat compared to open surgery or robotic-assisted laparoscopy (7-12). The main reasons for this are the commonly used two-dimensional imaging and the limited degrees of freedom available (13,14). While evidence for the benefits of three-dimensional imaging has already been presented (13,15-19), the practical benefits of laparoscopic instruments, which can perform three-dimensional movements, remain to be verified (20-24). Theoretically, the positive advantage of an added feature is clear. We may cite, for example, the flexible endoscope in single-incision multiport laparoscopic surgery, or the Kymerax© precision-drive articulating surgical system, which is advantageous in certain contexts, such as suturing at difficult angles and cutting along complex structures (22,25). Furthermore, the minimally invasive manipulator offers a cost-effective, non-robotic alternative for endoscopy (26). The positioning of the needle is one of the main difficulties in laparoscopic suturing (27,28). While the simplification of this surgical step would be welcomed, the question as to whether its theoretical benefits would be substantiated in practice remains to be answered. We selected a hand-operated needle holder with an additional rotation feature from Storz. Using a rotary control on the handle, it is possible to move the jaws and, consequently, the fixed needle can be rotated and positioned as appropriate to the circumstances (Figure 1). This study aimed to compare the rotational needle holder (RNH) from Storz with a conventional needle holder (CNH) from Storz (Figure 2A,B). For analysis of the operating devices, a simulation was used. The pelvitrainer has been proven effective in professional training, as well as in the evaluation of laparoscopic instruments (8,22). Using four simple tasks, we aimed to determine whether the RNH has advantages in terms of time, error rate, and precision. The four exercises tested suture competence at different angles in the direction of view. Furthermore, the participants’ subjective perceptions of the were determined using a questionnaire.

Methods
Study population
Due to the explorative nature of the evaluation, no setup was required for a formal number of cases. The study represents an initial evaluation of the RNH. A total of 23 participants were selected, all of whom were medical students at the University of Basel who had no prior laparoscopic experience. No left-handed students were recruited for the study. The ethics committee of Northwest and Central Switzerland (EKNZ) confirmed that the project is not defined as a research project according to Human Research Act Art. 2; therefore, IRB approval and written consent were not required.
Study design
All participants were assigned to two different groups. Group RC performed each task using the RNH first and subsequently using the CNH, while Group CR performed the tasks in reverse order. To enable the participants to become accustomed to laparoscopic conditions, one standardized identical instructional task was performed using the RNH and CNH. Subsequently, four tasks were performed using the RNH and CNH. The time taken, the overall precision, and the number of mistakes were recorded. After they had finished each exercise, the participants completed a questionnaire.
Instrument setup
A pelvitrainer with anatomical conditions was used for all exercises. It was full-featured with a 24-inch monitor and a 300W Xenon light source. For the imaging modality, a camera control unit with a capacity for recording videos of up to 720p resolution was installed. Two access points equivalent to the lateral ancillary trocar entry points were used for the needle holders. For the left hand, a CNH from Storz was available. The right hand had alternating access to the CNH and a needle holder with a normal up-righting function from Storz. The only variable that changed during testing was the needle holder (i.e., RNH or CNH).
Instruction
Initially, both needle holders were introduced and their functions explained. Thereafter, before each exercise, an introduction video was shown once to guarantee the reproducibility of the instruction. No questions were allowed. The participants were instructed to find the optimum combination in terms of precision, time, and errors. Precision and minimization of error are of utmost importance; however, efficiency is also crucial. To accustom the participants to the instruments and the pelvitrainer, an adaption task was performed in which the participants completed a simple task by grasping and fixating the needle, and attempting to form stitches.
Exercises
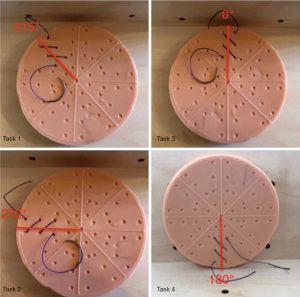
Tasks 1–4 were all suture tasks with the same fundamental principle. Each task consisted of three stitches from left to right or top down with a 20-cm long Variosoft 0 thread with a GS22 needle (Medtronic, Switzerland, Münchenbuchsee). The stitches were marked by two dots separated by a distance of 10 mm on silicone pads measuring 9×9 cm2. The pads had a consistency similar to that of a uterus. The individual tasks differed in one crucial aspect, namely, the angle in the direction of view. In the first exercise, the angle was 315° in the direction of view and horizontal to the ground; in the second, the angle was 270° (horizontal); in the third, the angle was 0° (horizontal); and the angle in the fourth exercise was 180° (vertically to the ground) (Figure 3). Each task was performed once with the CNH and RNH. Three different study parameters were measured: time taken, errors, and precision. Time was measured in minutes and seconds, and the maximum time allowed per exercise was 12 minutes. If the time limit was reached, the participant was obliged to cease work on the exercise instantly, but was not excluded. If the needle had been removed from the pad before the stitch was finished, this amounted to an error. Dropping the needle as part of the learning process did not count as a mistake. Precision was determined by measuring the deviation from the dot to the insertion and extraction points from the tip of the needle in millimetres. After each task, the participants were asked ten questions about their subjective perceptions of the exercise.
Questionnaire
The questionnaire comprised ten questions. The participants were asked the first five questions after each sequence of tasks:
- How would you describe the task’s difficulty level?
- Did you familiarize yourself with the instruments while performing the task?
- Did you familiarize yourself with the rotation function while performing the task?
- Did you perceive either of the needle holders to have any advantages over the other?
- Did you lose concentration at any point?
The participants answered the remaining five questions after they had used both devices to complete the exercises:
- Did the RNH simplify the tasks?
- Did the advantages (if applicable) of the RNH decrease over time?
- Was the rotational function intuitive?
- Would a neutral position of the rotational function improve its performance?
- Is there any other potential for improvement?
Statistical analysis
An explorative statistical analysis of the primary and secondary endpoints was carried out. To this end, a statistical evaluation of the 2×2 crossover was conducted using a linear mixed-effects model. The results were calculated as the average difference between the rotational and conventional techniques. Moreover, to adjust for a learning and sequence effect, a period and sequence effect was added to the design. The mean difference between time, precision, and errors between methods were evaluated with a 95% confidence interval and the corresponding P value. The questionnaire items were compared using McNemar’s test or the chi-squared test, as appropriate. A P value <0.05 was considered to be significant. All evaluations were performed using the statistical software R version 3.1.1 (29).
Results
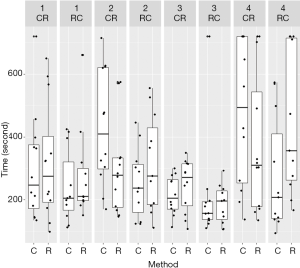
Task 1 was performed at a 315-degree horizontal angle. In terms of time, neither the methods nor comparison of the sequences and periods showed any significant difference (Figure 4). The same was true of the parameters’ precision and the occurrence of mistakes (Figures 5,6) (Table 1).
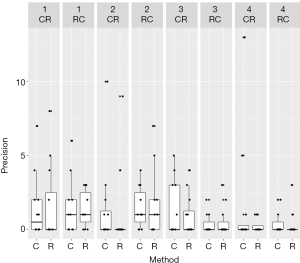
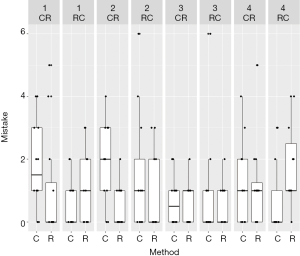
Table 1
| Parameter | Contrast | Collation | Difference | Lower CL | Upper CL | P value |
|---|---|---|---|---|---|---|
| Time | CR-RC | Sequence | 50.31 | −63.42 | 164 | 0.368 |
| 1-2 | Period | 9.186 | −69.36 | 87.73 | 0.8102 | |
| C-R | Method | −28.27 | −106.8 | 50.27 | 0.4625 | |
| Precision | CR-RC | Sequence | 0.09091 | −1.576 | 1.758 | 0.9108 |
| 1-2 | Period | −0.1288 | −0.8412 | 0.5836 | 0.7107 | |
| C-R | Method | −0.03788 | −0.7503 | 0.6745 | 0.913 | |
| Mistake | CR-RC | Sequence | 0.553 | −0.3547 | 1.461 | 0.219 |
| 1-2 | Period | 0.6439 | −0.1042 | 1.392 | 0.0879 | |
| C-R | Method | 0.1894 | −0.5588 | 0.9375 | 0.6041 |
C, conventional needle holder; R, rotational needle holder; CR-RC, the sequence, first with the conventional followed by the rotational needle holder
Task 2 was performed at a 270-degree horizontal angle: when utilizing the RNH, the participants made significantly fewer mistakes than when they used the CNH (P=0.003). This could not be confirmed in terms of difference between the sequences (P=0.961) or periods (P=0.200) (Figure 4). No apparent improvement in precision was observed (Figure 5). The participants finished the second period significantly faster (P=0.008); however, when compared with respect to the methods and sequences, the time difference was not significant (Figure 6) (Table 2).
Table 2
| Parameter | Contrast | Collation | Difference | Lower CL | Upper CL | P value |
|---|---|---|---|---|---|---|
| Time | CR-RC | Sequence | 78.17 | −33.14 | 189.5 | 0.159 |
| 1-2 | Period | 98.14 | 27.28 | 169 | 0.008959 | |
| C-R | Method | 35.86 | −35 | 106.7 | 0.3045 | |
| Precision | CR-RC | Sequence | −0.2955 | −2.291 | 1.7 | 0.7612 |
| 1-2 | Period | 0.2576 | −0.4142 | 0.9293 | 0.4341 | |
| C-R | Method | 0.07576 | −0.596 | 0.7475 | 0.8168 | |
| Mistake | CR-RC | Sequence | 0.02273 | −0.9512 | 0.9966 | 0.9618 |
| 1-2 | Period | 0.4318 | −0.2482 | 1.112 | 0.2008 | |
| C-R | Method | 1.068 | 0.3882 | 1.748 | 0.003685 |
C, conventional needle holder; R, rotational needle holder; CR-RC, the sequence, first with the conventional followed by the rotational needle holder
Task 3 was performed at a 0-degree horizontal angle: the students could not reduce the time required for the task by using the RNH (Figure 4). Precision and incidence of errors were not significantly improved by either method, period, or sequence (Figures 4-6; Table 3).
Table 3
| Parameter | Contrast | Collation | Difference | Lower CL | Upper CL | P value |
|---|---|---|---|---|---|---|
| Time | CR-RC | Sequence | 31.66 | −31.67 | 94.99 | 0.3103 |
| 1-2 | Period | −30.08 | −93.41 | 33.25 | 0.3346 | |
| C-R | Method | −2.258 | −65.59 | 61.07 | 0.9416 | |
| Precision | CR-RC | Sequence | 0.6705 | −0.2822 | 1.623 | 0.1581 |
| 1-2 | Period | 0.2992 | −0.3607 | 0.9592 | 0.3564 | |
| C-R | Method | 0.1174 | −0.5426 | 0.7774 | 0.7151 | |
| Mistake | CR-RC | Sequence | −0.1061 | −0.7627 | 0.5506 | 0.7403 |
| 1-2 | Period | −0.2273 | −0.8839 | 0.4293 | 0.4796 | |
| C-R | Method | 0.2273 | −0.4293 | 0.8839 | 0.4796 |
C, conventional needle holder; R, rotational needle holder; CR-RC, the sequence, first with the conventional followed by the rotational needle holder
Task 4 was performed at an 180-degree vertical angle: regarding the time required for task 4, no significant difference was observed between the methods (P=0.585) or sequences (P=0.336). It was clear that the students performed the task more efficiently during the second run, regardless of which technique was used (P=0.042) (Figure 4) (Table 4). No significant differences were observed with regard to precision or the incidence of errors. Neither was any significant difference observed between the exercises overall with respect to time taken, incidence of errors, or precision for either method.
Table 4
| Parameter | Contrast | Collation | Difference | Lower CL | Upper CL | P value |
|---|---|---|---|---|---|---|
| Time | CR-RC | Sequence | 65.59 | −73.1 | 204.3 | 0.3365 |
| 1-2 | Period | 134.6 | 5.114 | 264.1 | 0.04233 | |
| C-R | Method | −34.5 | −164 | 94.97 | 0.5853 | |
| Precision | CR-RC | Sequence | 0.5076 | −0.8627 | 1.878 | 0.4497 |
| 1-2 | Period | 0.6212 | −0.5602 | 1.803 | 0.2865 | |
| C-R | Method | 0.7121 | −0.4693 | 1.894 | 0.2238 | |
| Mistake | CR-RC | Sequence | −0.1061 | −0.9271 | 0.715 | 0.7908 |
| 1-2 | Period | 0.5455 | −0.2756 | 1.367 | 0.1816 | |
| C-R | Method | −0.5455 | −1.367 | 0.2756 | 0.1816 |
C, conventional needle holder; R, rotational needle holder; CR-RC, the sequence, first with the conventional followed by the rotational needle holder
Questionnaire results
According to the questionnaire’s results, most participants became accustomed to the equipment and to the rotational function after the first task. The students evaluated the level of difficulty of the tasks, giving average ratings of six and seven out of ten (1= easiest and 10= most difficult), except for task number 3, which was the easiest with an average rating of five out of ten. More than 65% of the participants had the impression that the RNH was advantageous in the first three exercises, and 87% of the participants expressed the same opinion in relation to task 2. Nevertheless, for the fourth challenge the majority saw no benefit. Less than 50% of the participants lost concentration during the practice, and 69.6% had the impression that the RNH was of benefit to them in performing the exercises, but that this effect decreased as they progressed through the tasks. The handling of the RNH was evaluated as counterintuitive by 69.6% of the students. All but one of the participants considered that a neutral position for the rotation function would be an advantage, and the majority thought that there was room for improvement in terms of the RNH’s manipulation.
Discussion
The purported benefits of the RNH are that it offers an improved learning curve and allows surgeons to work with greater speed, more accuracy, and fewer mistakes, resulting in a shorter operation time and cost reduction. In our study, the RNH increased the degrees of freedom relative to the needle. Because the results regarding the advantages and disadvantages of instruments with three-dimensional movement depend on the individual tool, we performed a randomized crossover study to validate the effectiveness of the RNH.
We anticipated that beginners in particular would benefit most from this technique, so in this study we chose participants who had no prior experience in laparoscopy. In principle, two techniques may be used to ensure the needle is at the appropriate angle in contact with the tissue: either the tissue is brought into the plane of the needle or the needle’s angle is adjusted with respect to the tissue. In our exercises, the latter procedure was necessary. We anticipated that the CNH would offer a clear advantage for this exercise. However, this could be only partially confirmed on the basis of our results. The data presented in Table 2 demonstrate that the second exercise with an angle of 270° was performed with the RNH with significantly fewer mistakes, and in the second period, significantly faster. Moreover, task 4 was performed faster during the second run, regardless of which technique was used. Neither of the other two tasks showed any significant difference (Tables 1,3), and overall comparison of all exercises revealed no significant difference between the two methods.
For all tested exercises, the participants performed the second round more efficiently. This may be attributed to a learning effect. To eliminate this bias, we conducted a crossover analysis. Additionally, the students improved their skills in tasks that included loading the needle on the needle holder, passing the needle through tissue, and manipulating the thread during suturing. Consequently, they performed each subsequent task more efficiently than the previous exercise. For the last exercise, which was more difficult, the participants needed more time (Figure 1). This was confirmed by the questionnaire results, wherein most of the participants reported that they became accustomed to the equipment after the first task and to the rotational function after the second task. Task 3 was rated easiest by most participants.
This study’s findings indicate that the RNH is superior to some extent, particularly for specific angles, but that this value is reduced for users with more experience and better laparoscopic skills. The results of the questionnaire supported this assessment and emphasized the counterintuitive handling of the RNH. Participants suggested that a neutral position for the rotation function would be superior. Laparoscopy continues to develop, and new methods, such as robot-assisted laparoscopy, improve the learning curve by simplifying execution and using superior equipment, including instruments that offer enhanced three-dimensional views, or laparoscopic devices with more degrees of freedom (5). However, these methods are cost intensive, and the outcomes have yet to be proven superior (30,31). Another strategy is to design mechanisms aimed at simplifying operational steps. For example, the laparoscopic stapler and the coagulation cutting instrument have gained wide appeal (32,33). The RNH is also designed to simplify an operational step, namely loading the needle. This study provides a first assessment of the rotational method. We recommend that the RNH be improved through a more intuitive execution of the needle holder. Future research should focus on whether experts profit from the rotational function, and whether it is associated with any difference in tissue loading. Incorrect placement of a curved needle leads to difficulty in driving the needle and, consequently, tissue force is drastically increased, in turn raising the risk of tissue rupture (34,35).
Procedures that are performed low in the pelvis at difficult angles for suture, such as sacrocolpopexy, could potentially benefit from a RNH with another degree of freedom. Comparison of this added degree of freedom and the superior three-dimensional view offered by robot-assisted laparoscopy is recommended as a topic for future studies.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: The authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ls.2019.11.03). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The ethics committee of Northwest and Central Switzerland (EKNZ) confirmed that the project is not defined as a research project according to Human Research Act Art. 2; therefore, IRB approval and written consent were not required.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Zhuang CL, Huang DD, Chen FF, et al. Laparoscopic versus open colorectal surgery within enhanced recovery after surgery programs: a systematic review and meta-analysis of randomized controlled trials. Surg Endosc 2015;29:2091-100. [Crossref] [PubMed]
- Schindlbeck C, Klauser K, Dian D, et al. Comparison of total laparoscopic, vaginal and abdominal hysterectomy. Arch Gynecol Obstet 2008;277:331-7. [Crossref] [PubMed]
- Aarts JW, Nieboer TE, Johnson N, et al. Surgical approach to hysterectomy for benign gynaecological disease. Cochrane Database Syst Rev 2015;12:CD003677 [PubMed]
- Berguer R, Rab GT, Abu-Ghaida H, et al. A comparison of surgeons' posture during laparoscopic and open surgical procedures. Surg Endosc 1997;11:139-42. [Crossref] [PubMed]
- Nezhat C, Saberi NS, Shahmohamady B, et al. Robotic-assisted laparoscopy in gynecological surgery. JSLS 2006;10:317-20. [PubMed]
- Zárate Rodriguez JG, Zihni AM, Ohu I, et al. Ergonomic analysis of laparoscopic and robotic surgical task performance at various experience levels. Surg Endosc 2019;33:1938-43. [Crossref] [PubMed]
- Callewaert G, Bosteels J, Housmans S, et al. Laparoscopic versus robotic-assisted sacrocolpopexy for pelvic organ prolapse: a systematic review. Gynecol Surg 2016;13:115-23. [Crossref] [PubMed]
- Chandra V, Nehra D, Parent R, et al. A comparison of laparoscopic and robotic assisted suturing performance by experts and novices. Surgery 2010;147:830-9. [Crossref] [PubMed]
- Jayaraman S, Quan D, Al-Ghamdi I, et al. Does robotic assistance improve efficiency in performing complex minimally invasive surgical procedures? Surg Endosc 2010;24:584-8. [Crossref] [PubMed]
- Doumerc N, Yuen C, Savdie R, et al. Should experienced open prostatic surgeons convert to robotic surgery? The real learning curve for one surgeon over 3 years. BJU Int 2010;106:378-84. [Crossref] [PubMed]
- McVey R, Goldenberg MG, Bernardini MQ, et al. Baseline Laparoscopic Skill May Predict Baseline Robotic Skill and Early Robotic Surgery Learning Curve. J Endourol 2016;30:588-92. [Crossref] [PubMed]
- Li XL, Du DF, Jiang H. The learning curves of robotic and three-dimensional laparoscopic surgery in cervical cancer. J Cancer 2016;7:2304-8. [Crossref] [PubMed]
- Leite M, Carvalho AF, Costa P, et al. Assessment of Laparoscopic Skills Performance: 2D Versus 3D Vision and Classic Instrument Versus New Hand-Held Robotic Device for Laparoscopy. Surg Innov 2016;23:52-61. [Crossref] [PubMed]
- Renda A, Vallancien G. Principles and advantages of robotics in urologic surgery. Curr Urol Rep 2003;4:114-8. [Crossref] [PubMed]
- Özsoy M, Kallidonis P, Kyriazis I, et al. Novice surgeons: do they benefit from 3D laparoscopy? Lasers Med Sci 2015;30:1325-33. [Crossref] [PubMed]
- Aykan S, Singhal P, Nguyen DP, et al. Perioperative, pathologic, and early continence outcomes comparing three-dimensional and two-dimensional display systems for laparoscopic radical prostatectomy--a retrospective, single-surgeon study. J Endourol 2014;28:539-43. [Crossref] [PubMed]
- Kim S, May A, Ryan H, et al. Distraction and proficiency in laparoscopy: 2D versus robotic console 3D immersion. Surg Endosc 2017;31:4625-30. [Crossref] [PubMed]
- Hagelsteen K, Langegård A, Lantz A, et al. Faster acquisition of laparoscopic skills in virtual reality with haptic feedback and 3D vision. Minim Invasive Ther Allied Technol 2017;26:269-77. [Crossref] [PubMed]
- Nishi M, Kanaji S, Otake Y, et al. Quantitative comparison of operative skill using 2- and 3-dimensional monitors during laparoscopic phantom tasks. Surgery 2017;161:1334-40. [Crossref] [PubMed]
- Ishimaru T, Takazawa S, Uchida H, et al. Development of a needle driver with multiple degrees of freedom for neonatal laparoscopic surgery. J Laparoendosc Adv Surg Tech A 2013;23:644-8. [Crossref] [PubMed]
- Takazawa S, Ishimaru T, Fujii M, et al. Assessment of suturing in the vertical plane shows the efficacy of the multi-degree-of-freedom needle driver for neonatal laparoscopy. Pediatr Surg Int 2013;29:1177-82. [Crossref] [PubMed]
- Sieber MA, Fellmann-Fischer B, Mueller M. Performance of Kymerax precision-drive articulating surgical system compared to conventional laparoscopic instruments in a pelvitrainer model. Surg Endosc 2017;31:4298-308. [Crossref] [PubMed]
- Di Lorenzo N, Camperchioli I, Gaspari AL. Radius surgical system and conventional laparoscopic instruments in abdominal surgery: application, learning curve and ergonomy. Surg Oncol 2007;16:S69-S72. [Crossref] [PubMed]
- Martinec DV, Gatta P, Zheng B, et al. The trade-off between flexibility and maneuverability: task performance with articulating laparoscopic instruments. Surg Endosc 2009;23:2697-701. [Crossref] [PubMed]
- Abe N, Takeuchi H, Ohki A, et al. Single-incision multiport laparoendoscopic surgery using a newly developed short-type flexible endoscope: a combined procedure of flexible endoscopic and laparoscopic surgery. J Hepatobiliary Pancreat Sci 2012;19:426-30. [Crossref] [PubMed]
- Bosma J, Aarts S, Jaspers J. The minimally Invasive Manipulator: an ergonomic and economic non-robotic alternative for endoscopy? Minim Invasive Ther Allied Technol. 2015;24:24-30. [Crossref] [PubMed]
- Waseda M, Inaki N, Torres Bermudez JR, et al. Precision in stitches: Radius Surgical System. Surg Endosc 2007;21:2056-62. [Crossref] [PubMed]
- Brody F, Rehm J, Ponsky J, et al. A reliable and efficient technique for laparoscopic needle positioning. Surg Endosc 1999;13:1053-54. [Crossref] [PubMed]
- R Development Core Team. R: A language and environment for statistical computing. R Foundation for R Statistical Computing 2015.
- Sarlos D, Kots L, Stevanovic N, et al. Robotic hysterectomy versus conventional laparoscopic hysterectomy: outcome and cost analyses of a matched case-control study. Eur J Obstet Gynecol Reprod Biol 2010;150:92-6. [Crossref] [PubMed]
- Desille-Gbaguidi H, Hebert T, Paternotte-Villemagne J, et al. Overall care cost comparison between robotic and laparoscopic surgery for endometrial and cervical cancer. Eur J Obstet Gynecol Reprod Biol 2013;171:348-52. [Crossref] [PubMed]
- Gözen AS, Teber D, Rassweiler JJ. Principles and initial experience of a new device for dissection and hemostasis. Minim Invasive Ther Allied Technol 2007;16:58-65. [Crossref] [PubMed]
- Yao DB, Wu SD. Application of stapling devices in liver surgery: Current status and future prospects. World J Gastroenterol 2016;22:7091-8. [Crossref] [PubMed]
- Hernandez R, Onar-Thomas A, Travascio F, et al. Attainment and retention of force moderation following laparoscopic resection training with visual force feedback. Surg Endosc 2017;31:4805-15. [Crossref] [PubMed]
- Hardon SF, Horeman T, Bonjer HJ, et al. Force-based learning curve tracking in fundamental laparoscopic skills training. Surg Endosc 2018;32:3609-21. [Crossref] [PubMed]
Cite this article as: Zwimpfer TA, Fellmann-Fischer B, Oehler R, Schötzau A, Kind AB. A crossover study on the advantage of an additional rotation function in a needle holder compared to a conventional needle holder in a pelvitrainer model. Laparosc Surg 2020;4:10.