
Retrospective evaluation of the crucial factor in total laparoscopic hysterectomy by using video review
Introduction
Hysterectomy is a common gynecological surgery performed for uterine myomas, uterine cancers, and uterine prolapses. It can be performed using various techniques: abdominal hysterectomy, vaginal hysterectomy, laparoscopic hysterectomy, and robotic-assisted laparoscopic hysterectomy. Endoscopic surgery, particularly laparoscopy, has been increasingly chosen as the surgical method for gynecological diseases because minimally invasive surgery with the development of technique and instruments would result in decreased hospitalization period.
In 2016, 67,758 cases of laparoscopic surgery were performed at 440 facilities in Japan, of which 16,940 procedures (25.0%) were total laparoscopic hysterectomy (TLH) (1). The procedures in TLH are essential as the basis for performing other gynecological laparoscopic surgeries. Till now, there have been few reports with regard to the learning curve for TLH. In addition, the experiences and skills of individual gynecologists for performing TLH have not been evaluated (2). Therefore, we sought to define the technical problems and the rate-limiting steps regarding the learning tasks to improve the surgical skills by the evaluation on several steps and recording the changes in the surgical time.
Methods
We reviewed retrospectively the videos and clinical records of patients who underwent TLH for benign diseases from June 2017 to September 2018 at Japanese Red Cross Yamaguchi Hospital. The procedure was performed mainly by a single gynecologist who had continued the dry box-training. We assessed a total of 30 TLH cases. Written informed consent was obtained from all participants, and the study was approved by the institutional review board (IRB number: H30-16).
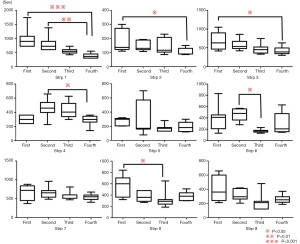
We divided the procedure of TLH into the following nine steps: step 1, pneumoperitoneum for the initiation of the operation; step 2, the setting of all laparoscopic ports into the abdominal cavity; step 3, the identification of ureter and the transection of uterine artery; step 4, the transection of the adnexa (infundibulopelvic or utero-ovarian ligament) and the retroperitoneum heading to the uterosacral ligament; step 5, the dissection of parametrium; step 6, the execution of colpotomy; step 7, the closure of vaginal cuff by suturing; step 8, hemostasis and retroperitoneal suture; and step 9, observation of the abdominal cavity till the end.
The operation period was arbitrarily classified into the four phases (phases 1, 2, 3, and 4) from the beginning phase to the last. For each of the former three phases, 7 cases were assigned. For phase 4, 9 cases were allocated. The standard technique for TLH at our institution is as follows: as the open method, a 12-mm camera trocar is placed, and other trocars (5 mm) are set in a diamond shape. The cavity between bladder and uterus, peritoneum, and the anterior portions of broad ligament are appropriately opened, and the round ligament is cut. Each ureter is identified, and the uterine artery is ligated by using the absorbable threads. Next, the adnexa and retroperitoneum are transected, and the parametrium is dissected. Then, colpotomy is performed, the vaginal cuff is closed, and hemostasis is achieved along with retroperitoneal suture. An anti-adhesion agent is applied, all trocars are removed, the wound is closed, and urine flow through the ureteral orifice is confirmed with a cystoscope.
All statistical analyses were performed using Graphpad Prism version 5 (GraphPad Software Inc., San Diego, CA, USA). We performed repeated-measures analysis of variance (Kruskal-Wallis test) to investigate the significance of differences between the four phases; the correlation matrix and multiple regression analysis were also constructed to determine whether any of the steps [1–9] were correlated. A P value of 0.05 was considered statistically significant.
Results
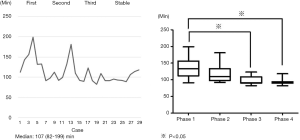
Median age of patients was 46 years (range, 39–69 years), and median body mass index was 21.1 kg/m2 (range, 16.9–27.4 kg/m2). There were no complications during the perioperative period (Table 1). Almost surgeries, 28 (93.3%) of the 30 cases, were performed for uterine myoma. Median surgical time, blood loss amount, and uterine weight were 107 min (range, 82–199 min), 5 mL (range, 5–350 mL), and 241 g (range, 47–971 g), respectively. There were no differences in patient characteristics (age, body mass index, parity, and uterine weight) among the four phases. The total surgical time for phase 3 was significantly shorter than that for phase 1 (P<0.05; Figure 1). The technique of TLH gradually stabilized by phase 3. Surgical time positively correlated with uterine weight (P=0.0346, R=0.1875) and amount of blood loss amount (P=0.0001, R=0.4755), whereas no significant correlation was noted between uterine weight and blood loss amount (Figure 2A).
Table 1
| Characteristics | n |
|---|---|
| Number | 30 |
| Age in years (range) | 46† [39–69] |
| Body mass index in kg/m2 [range] | 21.1† [16.9–27.4] |
| History of abdominal surgery | |
| Yes | 7 |
| No | 23 |
| Parity | |
| 1 or more | 25 |
| 0 | 5 |
| Disease | |
| Uterine myoma | 28 |
| Abnormal cytological findings | 2 |
| Uterine weight in grams [range] | 241† [47–971] |
†, value shown is the median.
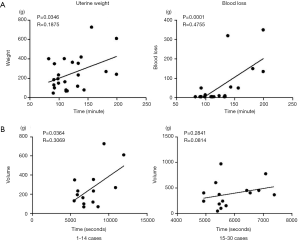
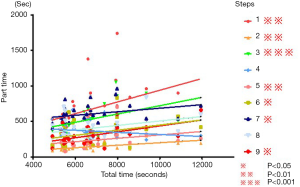
Further, among the latter 15 cases in phases 3 and 4, there were no significant differences between uterine weight and surgical time (Figure 2B). Time courses of steps 1, 2, and 3 of phase 4 were significantly shorter than those of phase 1 (P<0.01 for all; Figure 3). The most crucial factor affecting the surgical time in TLH was observed to be the identification of ureter and the transection of uterine artery (P<0.001; Figure 4).
Discussion
With being spreading the gynecological endoscopic surgery, the surgical skills in TLH are needed for various kinds of laparoscopic operations. In this study, we assessed the rate-limiting step in TLH, and found that the total surgical time was strongly influenced by the step including the identification of ureter and the transection of uterine artery. Based on the several information regarding the patient, the surgeons need to consider the approach for hysterectomy. In cases of nulliparity, previous surgeries, and severe endometriosis, an abdominal or laparoscopic approach is usually preferred, whereas multiparity and uterus with small size and descent are often approached vaginally.
A surgeon without the sufficient experiences in TLH would have difficulty of identifying the uterine artery, superficial uterine vein, upper bladder artery, and other structures in pelvic cavity. In case of occurring the bleeding by the damage on small vessels around the ureter, it would be difficult to have the fine operative field. Consequently, the surgical time is possibly extended. When the gynecologists with insufficient experience of performing TLH, it might need the prolonged time to identify the ureter, no matter how frequently they train in a dry box. In contrast, several surgeons have recently suggested that, the identification of ureter in TLH for benign disease would be unnecessary to complete the surgery. Although we want to emphasize the importance of this step as the ideal one, if this procedure is not needed, the total surgical time can be shortened.
There have previously been few reports with regard to the learning curve for TLH. In one study of TLH performed through only a single port, the time for vaginal suturing was obviously shortened after completing 20 cases, and the total surgical time was shortened after 40 cases (3). Reade et al. reported that the learning curve for TLH improved after the experience of 23 cases (4). Their techniques of “buddy operating,” in which two surgeons combined referrals and operated together, increased the rate of skill acquisition. Donnez and Donnez described that laparoscopic hysterectomy must be the superior technique, particularly in view of the low rates of urinary tract complications achieved by appropriately trained surgeons (5).
In 2018, the robotic-assisted surgery for benign uterine disease was approved for the health insurance coverage in Japan. There are some common characteristics between robotic and laparoscopic surgery, such as the use of combination of the field of view from the scope and hand-eye coordination. However, there are individual differences in the abilities of gynecologists, i.e., hand-eye coordination and spatial recognition techniques. The learning curve for robotic surgery has been discussed worldwide (6,7). For the surgeons with advanced surgical skills in laparoscopic robotic operations, it was mentioned that the operative times stabilize after 50 cases (6). Sandadi et al. suggested that at least 50 total cases were required to become proficient in robotic hysterectomy (7). However, in our study, the surgical time stabilized by phase 3, suggesting that TLH is different from robotic-assisted surgery, and it is possible to learn early. Conversely, Lim et al. (8) reported that learning to perform robotic-assisted hysterectomy with lymph node dissection seems easier than learning to perform laparoscopic hysterectomy for the surgical management of endometrial cancer. Akdemir et al. showed that an experienced robotic surgeon requires approximately 14 procedures to achieve proficiency in intracorporeal cuff suturing during robotic single-site total hysterectomy (9). The console stage of the main robotic surgery seems to be learned most rapidly, whereas the stage for suturing shows the slowest learning curve (10). Robotic surgery and laparoscopic surgery have different console times; thus, they cannot be unconditionally compared.
A 2008 report indicated that TLH for uterine malignant tumors can be safely implemented (11). In 2016, the rates of surgery performed for malignant tumor was approximately 5.2% in a total 67,758 cases of laparoscopic operation because of the problems involving standardization of adaptation, procedures, and operator training in Japan. Although laparoscopic surgery for uterine malignant tumors has been increasing in recent years, identification of the ureter and transection of uterine artery are indispensable when performing semi-radical hysterectomy. We think that necessary information regarding TLH should be acquired to perform laparoscopic surgery safety and appropriately for patients with uterine cancer.
To the best of our knowledge, evaluation of the crucial factors in TLH has not been reported to date. We found that the identification of the ureter and the transection of the uterine artery influenced the total surgical time. Further studies are needed to assess whether these data will be applicable to other surgeons.
Conclusions
TLH comprises many steps that involve multiple techniques. The steps involving the identification of the ureter and the transection of the uterine artery may affect the total surgical time. We hope these data will help young obstetricians/gynecologists to perform TLH safely and promptly.
Acknowledgments
Enago provided language help, writing assistance, and proofreading services for this article. We would like to express our sincere gratitude to them.
Funding: None.
Footnote
Conflicts of Interest: The authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ls.2019.05.05). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the institutional review board (IRB number: H30-16) and written informed consent was obtained from all patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Taniguchi F, Wada-Hiraike O, Hirata T, et al. A nationwide survey on gynecologic endoscopic surgery in Japan, 2014-2016. J Obstet Gynaecol Res 2018;44:2067-76. [Crossref] [PubMed]
- Kreiker GL, Bertoldi A, Larcher JS, et al. Prospective evaluation of the learning curve of laparoscopic-assisted vaginal hysterectomy in a university hospital. J Am Assoc Gynecol Laparosc 2004;11:229-235. [Crossref] [PubMed]
- Paek J, Kim SW, Lee SH, et al. Learning curve and surgical outcome for single-port access total laparoscopic hysterectomy in 100 consecutive cases. Gynecol Obstet Invest 2011;72:227-33. [Crossref] [PubMed]
- Reade C, Hauspy J, Schmuck ML, et al. Characterizing the learning curve for laparoscopic radical hysterectomy: buddy operating as a technique for accelerating skill acquisition. Int J Gynecol Cancer 2011;21:930-5. [Crossref] [PubMed]
- Donnez O, Donnez J. A series of 400 laparoscopic hysterectomies for benign disease: a single centre, single surgeon prospective study of complications confirming previous retrospective study. BJOG 2010;117:752-5. [Crossref] [PubMed]
- Lenihan JP Jr, Kovanda C, Seshadri-Kreaden U. What is the learning curve for robotic assisted gynecologic surgery? J Minim Invasive Gynecol 2008;15:589-94. [Crossref] [PubMed]
- Sandadi S, Gadzinski JA, Lee S, et al. Fellowship learning curve associated with completing a robotic assisted total laparoscopic hysterectomy. Gynecol Oncol 2014;132:102-6. [Crossref] [PubMed]
- Lim PC, Kang E, Park DH. Learning curve and surgical outcome for robotic-assisted hysterectomy with lymphadenectomy: case-matched controlled comparison with laparoscopy and laparotomy for treatment of endometrial cancer. J Minim Invasive Gynecol 2010;17:739-48. [Crossref] [PubMed]
- Akdemir A, Zeybek B, Ozgurel B, et al. Learning curve analysis of intracorporeal cuff suturing during robotic single-site total hysterectomy. J Minim Invasive Gynecol 2015;22:384-9. [Crossref] [PubMed]
- Tang FH, Tsai EM. Learning curve analysis of different stages of robotic-assisted laparoscopic hysterectomy. Biomed Res Int 2017;2017:1827913 [Crossref] [PubMed]
- Andrea JG, Marcelo Carraro N. Total laparoscopic hysterectomy: The Brisbane learning curve. Aust N Z J Obstet Gynaecol 2007;47:65-9. [Crossref] [PubMed]
Cite this article as: Komatsu H, Taniguchi F, Nagata H, Nakaso T, Nagaya Y, Tsukihara S, Sarugami M, Harada T, Kanamori Y. Retrospective evaluation of the crucial factor in total laparoscopic hysterectomy by using video review. Laparosc Surg 2019;3:23.


