A balancing act: obstruction following laparoscopic closure of a congenital paraduodenal hernia
Introduction
Left paraduodenal hernias (LPDH) are formed embryologically when the mesenteric and parietal peritoneum fail to fuse and can be associated with malrotation of the midgut. A hernia sac containing varying amounts of small bowel is thus formed in Landzert’s space (1). Left paraduodenal hernias, the more common type, constitute more than 40% of congenital internal hernias (1). However, they remain a rare entity, with only 50 case reports published between 1980 and 2017 (2). Patients are typically diagnosed later in life, commonly between the fourth and sixth decades, after presenting with acute symptoms. However, 50% of patients describe more chronic abdominal pain when prompted (3). Computed tomography (CT) is the best imaging modality to diagnose LPDH, showing the typical appearance of a cluster of dilated loops of small bowel to the left of the ligament of Treitz, with mass effect causing displacement of the posterior wall of the stomach, duodenal flexure, and transverse colon inferiorly. The inferior mesenteric vessels appear engorged and stretched at the entrance of the hernia sac (4). Surgical repair is recommended, regardless of symptoms, given the risk of obstruction and strangulation. Furthermore, when patients present with a strangulated paraduodenal hernia, their mortality rate approaches 50% (5). The standard approach is reduction of the hernia sac contents with closure of the defect. Laparoscopic repair has gained popularity over the past decade, however most authors advocate for an open approach when the patient presents acutely due to the risk of strangulated bowel (2).
Case presentation
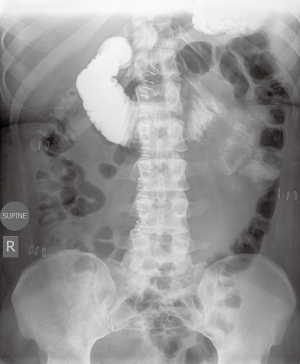
This patient is a 22-year-old woman with no prior abdominal operations, who presented with one day of left lower abdominal pain and emesis. She described the pain as relentless and “the worst pain of my life”, associated with non-bilious emesis. The patient had been experiencing postprandial discomfort after eating over the past year. She presented with a leukocytosis of 14.6K and a left shift. Her abdominal exam was notable for tenderness in the left upper and, to a lesser extent, left lower quadrant without physical exam findings of peritonitis. CT scan (Figure 1) revealed a sac-like configuration of small bowel through a mesenteric defect in the left anterior para-renal orifice. Given the concern for a paraduodenal hernia with bowel ischemia, she underwent emergent laparoscopic reduction of this internal hernia and closure of the defect using Endo StitchTM (Medtronic, Fridley, United States) sutures (Figure 2).
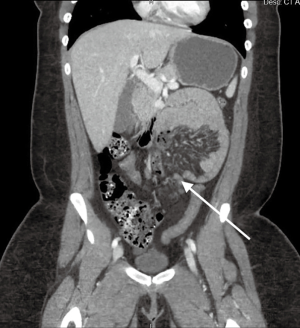

The patient was discharged home two days after the operation, eating a regular diet. On post-operative day 14, she presented to the emergency department due to increasing abdominal pain and bilious emesis. She reported feeling well and tolerating a diet up until that day. On exam, she appeared distressed and was moderately distended with severe generalized tenderness. CT scan showed a high-grade small bowel obstruction at the distal duodenum with proximal duodenal and stomach dilation, without evidence of bowel ischemia. She was taken emergently for a diagnostic laparoscopy, which revealed grossly dilated bowel and edematous injected mesentery with the transition point at the previously closed hernia defect. The decision was made to convert to a laparotomy given the extensive scarring leading to an inability to identify the sutures closing the previous defect. Once open, two of the sutures, compressing the bowel at the ligament of Treitz, were removed. Insufflated air via an orogastric tube confirmed that air easily passed through to the distal bowel, leading to normal distension. Her post-operative course was uncomplicated. An upper gastrointestinal (UGI) series (Figure 3) showed no mechanical obstruction. At one-month follow-up, the patient was doing well had no problems with eating.
Discussion
We present a case of a patient with a LPDH who underwent laparoscopic repair, which was complicated by obstruction due to a hernia closure that was too tight. The time course of her subsequent presentation (14 days after initial operation) was likely due to the timing of the scarring of the mesentery around the bowel at the site of the closure. To date, there have been no case reports detailing this type of complication. It is important for adult general surgeons who may see this rare pathology only a few times in their career to be cognizant of this possibility. The defect needs to closed adequately to avoid recurrence of internal hernia, but not too tight, causing narrowing of the proximal jejunum and leading to bowel obstruction. In order to prevent the latter complication, we recommend an intraoperative air test using orogastric tube to insufflate the bowel to ensure that the patency of the bowel after closure of the defect. Furthermore, an UGI should be done prior to discharge to identify any significant narrowing of the bowel. Finally, any patient who presents with a bowel obstruction after repair of a LPDH should be evaluated promptly, with a low threshold to proceed to the operating room.
Acknowledgments
We would like to thank our patient for agreeing to share her story.
Funding: None.
Footnote
Conflicts of Interest: The authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ls.2019.07.05). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Declaration of Helsinki (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Al-Khyatt W, Aggarwal S, Birchall J, et al. Acute intestinal obstruction secondary to left paraduodenal hernia: a case report and literature review. World J Emerg Surg 2013;8:5. [Crossref] [PubMed]
- Kozman MA, Fisher OM. Left Paraduodenal Hernia: A Rare Complication following Laparoscopic Appendectomy. Case Rep Surg 2017;2017:3913784 [Crossref] [PubMed]
- Gusz JR, Wright LM. Intestinal obstruction secondary to left paraduodenal hernia. J Surg Case Rep 2015;2015: [Crossref] [PubMed]
- Takeyama N, Gokan T, Ohgiya Y, et al. CT of internal hernias. Radiographics 2005;25:997-1015. [Crossref] [PubMed]
- Shi Y, Felsted AE, Masand PM, et al. Congenital left paraduodenal hernia causing chronic abdominal pain and abdominal catastrophe. Pediatrics 2015;135:e1067-71. [Crossref] [PubMed]
- Pulcrano ME, Vu L, Lin MC. Using a laparoscopic approach, the ligament of Treitz was located and the hernia was then identified. Asvide 2019;6:224. Available online: http://www.asvide.com/watch/32909
Cite this article as: Pulcrano ME, Vu L, Lin MC. A balancing act: obstruction following laparoscopic closure of a congenital paraduodenal hernia. Laparosc Surg 2019;3:35.