
Laparoscopic hepatic resection
IntroductionOther Section
- Introduction
- Background
- Definitions
- Patient selection—start with the easy ones
- Instrumentation
- Anesthesia & pneumoperitoneum
- Bleeding
- Individual operations
- Evidence
- Conclusions
- Acknowledgments
- Footnote
- References
For many years, open liver resection has been considered a difficult and risky procedure, mostly because of the often complex anatomy of the liver and the high incidence of bleeding problems. Improvements in technique and instrumentation saw a dramatic decline in mortality in open resection over the 1970’s and 1980’s (1). Laparoscopic abdominal surgery became widespread in the 1990s but took some time to become adapted to laparoscopic liver resection (LLR) (2). The main barriers were fear of bleeding, difficult access and inadequate instrumentation.
Sporadic reports appeared in the mid 1990s, but it was the seminal paper and dramatic video presentations of Cristiano Hüscher which inspired surgeons throughout the world to take up the challenge and perform major resection laparoscopically (3).
The last two decades have seen a dramatic increase in LLR, although the degree of enthusiasm varies from center to center and country to country. At the time of publication, Suh and colleagues have reported over 700 pure laparoscopic donor hepatectomies from a multicenter experience in Korea (4). Regarding LLR, there is now level I evidence that LLR can be safer with less blood loss and shorter hospital stays with similar oncologic outcomes compared to open liver surgery (5,6). In this paper, we explore some of the developments of laparoscopic hepatic resection and hope to bring the reader up to date with current best practice.
BackgroundOther Section
- Introduction
- Background
- Definitions
- Patient selection—start with the easy ones
- Instrumentation
- Anesthesia & pneumoperitoneum
- Bleeding
- Individual operations
- Evidence
- Conclusions
- Acknowledgments
- Footnote
- References
Liver surgery is not like other surgery. There are wide variations in the degree of difficulty depending on the location of the tumors as well as the amount of liver to be resected. Minor resections can be simple and straightforward whereas more complex resections carry significant risks. International descriptions of actual operations varied to such an extent that the nomenclature was redefined at the Brisbane IHPBA conference in 2000 (7). Numerous experts in open hepatic surgery devised a framework of anatomical description, the segments of the liver and also defined the operations in an attempt to standardize surgical reporting worldwide. It is interesting to note that at this international liver meeting in the year 2000, there were no invited presentations on laparoscopic liver surgery.
Following sporadic reports from Japan and Europe and subsequently Hüscher’s work, LLR gained momentum in several centers (8-11). There was some reluctance from traditional open liver surgeons to take on the new techniques, especially when they had no laparoscopic “training” operations such as cholecystectomy, appendicectomy and hernia repair. This meant that many early published series came from smaller liver units where general surgery was also practiced (12).
In the 2000s, there was a rapid increase in reporting of LLR with our own paper on laparoscopic right hepatectomy appearing in 2004 (13). David Geller has chronicled that early publication explosion documenting 2,800 reported cases in 2009 (14). This was followed by Ruben Ciria and others reporting 9, 000 cases in 2016 (15).
This enthusiasm for LLR was corralled by Joe Buell from Louisville, Kentucky where the first international consensus meeting of LLR was held in 2008 with great success (16) (Figure 1). Go Wakabayashi organized a second international consensus meeting in 2014 in Morioka, Japan (17). The consensus statements from both these meetings have been widely cited. The need for ongoing organization of surgeons interested in LLR led to the formation of a group dedicated to its demonstration and teaching. The International Laparoscopic Liver Society (ILLS) was officially formed in 2016 in Sao Paulo, Brazil at the IHPBA meeting with Daniel Cherqui as the first president (18). The first stand-alone meeting was held in Paris in 2017 and the second in Tokyo in 2019. Future meetings are planned for New York in 2021 and Rome, Italy in 2023.

DefinitionsOther Section
- Introduction
- Background
- Definitions
- Patient selection—start with the easy ones
- Instrumentation
- Anesthesia & pneumoperitoneum
- Bleeding
- Individual operations
- Evidence
- Conclusions
- Acknowledgments
- Footnote
- References
Laparoscopic liver surgery has been defined as pure, hybrid, hand-assisted or converted. Pure LLR implies that liver mobilization and parenchymal transection are all performed using laparoscopic instrumentation. The hybrid approach implies a combination of open and laparoscopic techniques such as laparoscopic liver mobilization and a right upper quadrant incision to aid liver parenchymal transection. Hand-assisted techniques involve the use of a gel hand port, through which either a surgeons or assistants hand can be placed inside the abdomen to manipulate the liver and assist mobilization and parenchymal dissection. A conversion is where a formal laparotomy is required to complete an operation because of technical or oncological issues hindering surgical progression.
Patient selection—start with the easy onesOther Section
- Introduction
- Background
- Definitions
- Patient selection—start with the easy ones
- Instrumentation
- Anesthesia & pneumoperitoneum
- Bleeding
- Individual operations
- Evidence
- Conclusions
- Acknowledgments
- Footnote
- References
Advocates of LLR have demonstrated that young women without fatty liver disease tend to have slim livers, with parenchyma which is easy to transect. In contrast, obese males with stiff fatty livers will of course be more technically challenging. The presence of cirrhosis infers similar contraindications to resection as in open surgery. Some authors have recently postulated that when surgery is necessary, laparoscopic resection is safer than an open approach for Child’s B cirrhotics (19). There is less abdominal wall disruption and reduced ascites following LLR in cirrhotic patients.
Many authors have published on the need for a stepwise graduated development of an individual's operative experience because of the laparoscopic learning curve (20,21). Readers are directed to the IWATE scoring system, first described by Go Wakabayashi (22). It is recommended that surgeons at the beginning of their learning curve begin with favorable small peripheral lesions in easily accessible locations before progressing to left lateral sectionectomy (Figure 2). Formal left hepatectomy can be followed by right hepatectomy and then surgery of a more complex nature, particularly removal of segments VII and VIII.
InstrumentationOther Section
- Introduction
- Background
- Definitions
- Patient selection—start with the easy ones
- Instrumentation
- Anesthesia & pneumoperitoneum
- Bleeding
- Individual operations
- Evidence
- Conclusions
- Acknowledgments
- Footnote
- References
Instrumentation varies from surgeon to surgeon in LLR just as it does in open surgery. The techniques of parenchymal transection remain the most varied and debated due to differences in surgeon’s preferences. The trend for linear stapling alone seems to have faded because of the occasional major hemorrhage that can follow. Most surgeons prefer more precise and controlled methods of transection using devices such as Harmonic Shears® (Ethicon Endo-Surgery, Cincinnati, OH, USA), LigasureTM (Medtronic, Norwalk, CT, USA), and Enseal® (Ethicon Endo-Surgery, Cincinnati, OH, USA); with CUSATM (Cavitron Ultrasonic Surgical Aspirator, Tyco Healthcare, Mansfield, MA, USA) for more precise scalloping of the liver surface close to large traversing vessels. Linear staplers such as Endo GIATM (Medtronic, Norwalk, CT, USA) or the new Echelon FlexTM (Ethicon Endo-Surgery, Cincinnati, OH, USA) powered vascular stapler (PVS) from Ethicon remain very useful for controlling bleeding from large vessels and leakage from bile ducts (23). Since inception, laparoscopic ultrasound is now considered essential in modern day LLR. It allows the surgeon to be confident of tumor margins, while defining anatomy with more precision (24). Its use in tumor detection is somewhat limited in patients with fatty liver disease, severe cirrhosis or peliosis.
Anesthesia & pneumoperitoneumOther Section
- Introduction
- Background
- Definitions
- Patient selection—start with the easy ones
- Instrumentation
- Anesthesia & pneumoperitoneum
- Bleeding
- Individual operations
- Evidence
- Conclusions
- Acknowledgments
- Footnote
- References
A dedicated liver anesthetist is helpful when performing open or LLR. As in open surgery, a low central venous pressure is essential to reduce venous bleeding (25). The addition of pneumoperitoneum also appears to confer benefit by reducing bleeding (26,27). Surgeons argue about the ideal carbon dioxide pressure, with levels between 10 and 20 mmHg being reported (28). Pneumoperitoneum can lead to gas embolism, especially when large hepatic veins are entered. Carbon dioxide embolism is much safer than air embolism because carbon dioxide dissolves 50 times faster than nitrogen. As yet there remains no documented mortality from carbon dioxide embolism in LLR.
Some surgeons raise the pressure to as high as 20 mmHg when bleeding occurs. As Honda and his group have pointed out, the intrathoracic pressure controlled by the anesthetist can also affect venous pressure and hepatic bleeding (29). This can only be negated by dropping this positive pressure and when major hemorrhage occurs, Honda suggests that all mechanical ventilation should be ceased for three minutes to enhance control of venous bleeding.
BleedingOther Section
- Introduction
- Background
- Definitions
- Patient selection—start with the easy ones
- Instrumentation
- Anesthesia & pneumoperitoneum
- Bleeding
- Individual operations
- Evidence
- Conclusions
- Acknowledgments
- Footnote
- References
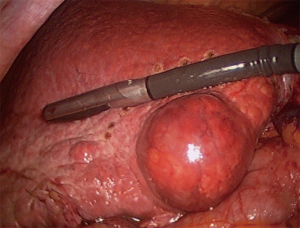
Unexpected bleeding during LLR can be frightening. Most surgeons agree it is best controlled laparoscopically rather than converting. Laparoscopic suturing skills are essential when taking on more advanced liver resections. A thorough understanding of intrahepatic anatomy is essential before tackling major laparoscopic hepatectomy. This anatomic understanding can come from practising open surgery or training with others doing laparoscopic liver surgery (30,31). The Pringle maneuver of inflow occlusion to the whole liver is back in fashion (Figure 3). Temporary hepatic inflow occlusion reduces bleeding and with judicious use appears to have little harmful effect on the liver (32).

Individual operationsOther Section
- Introduction
- Background
- Definitions
- Patient selection—start with the easy ones
- Instrumentation
- Anesthesia & pneumoperitoneum
- Bleeding
- Individual operations
- Evidence
- Conclusions
- Acknowledgments
- Footnote
- References
Non-anatomical wedge resections usually require intraoperative laparoscopic USS to confirm the margin and are usually straightforward when undertaken in segments II, III, IVB, V and VI. The patient’s positioning is important for right sided lesions where the left lateral position (right side up) is helpful. Lesions in segment VII and VIII can be hard to see and usually require full right lobe mobilization. Resection can be assisted by intercostal and even transthoracic trocars (33).
Left lateral sectionectomy is almost too easy but at least one mortality has occurred without publication. The parenchyma can be divided anteriorly with an energy device and staplers can be used to control both inflow and outflow. Formal left hepatectomy is more challenging and brings on the option of Glissonian dissection of the inflow versus individual vessel ligation. For lesions well clear of the inflow structures, Glissonian dissection is reasonable. It can be difficult to stay outside the sheath but just as in open surgery, reports from Japan have encouraged its use (34).
For right hepatectomy, the caudal approach of Soubrane or the recently presented modified dorsal approach by Bryant offer elegant methods of exposing the porta by extended caudate division (35,36). The liver must be mobilized off the vena cava and the right hepatic vein can be divided inside or outside the liver. Once again, surgical opinion varies regarding the benefits of Glissonian over individual vessel ligation. The Japanese in particular have taken Glissonian dissection to a higher level with Go Wakabayashi reporting intricate hilar exposure of the inflow to all four segments (37).
Laparoscopic living donor hepatectomy was first described by Cherqui et al. for a left lateral segment from parent to child in 2002 (38). Subsequent reports by Kwon, Han and others surprised the world with pure laparoscopic right lobe donation (39,40). This procedure has become almost standard in Korea where several centers have reported over one hundred cases without mortality.
EvidenceOther Section
- Introduction
- Background
- Definitions
- Patient selection—start with the easy ones
- Instrumentation
- Anesthesia & pneumoperitoneum
- Bleeding
- Individual operations
- Evidence
- Conclusions
- Acknowledgments
- Footnote
- References
Many individual series and case control series have reported lower morbidity and equivalent oncological outcomes when comparing LLR to open resection. Several centers, including ours, have used propensity scores to more accurately compare cohorts of patients undergoing resection for colorectal metastases. Once again, less short-term morbidity, and similar oncologic outcomes have been reported (5,41,42).
A recent, well run randomized trial from Oslo, Norway has shown improved short-term outcomes with LLR vs. open (6). Their study randomized 250 patients with colorectal metastases who needed resection of three hepatic segments or less. Bleeding was similar, morbidity was less, and hospital stay was shorter. They have recently published the oncological outcomes and demonstrated equivalence (43). For hepatocellular cancer, a propensity score analysis from Japan has shown improved morbidity and similar survival curves (44). A small randomized trial from Egypt has shown better short-term outcomes for hepatocellular carcinoma when done laparoscopically (45). The ORANGE II PLUS trial run by Ronald Van Dam from Maastricht in Holland is an international multicenter randomized controlled trial comparing open versus laparoscopic right hemihepatectomy (46). Patient accrual is complete, and results are eagerly awaited.
ConclusionsOther Section
- Introduction
- Background
- Definitions
- Patient selection—start with the easy ones
- Instrumentation
- Anesthesia & pneumoperitoneum
- Bleeding
- Individual operations
- Evidence
- Conclusions
- Acknowledgments
- Footnote
- References
LLR has been increasing worldwide. Many centers are performing minor resections. More and more units are undertaking major hepatectomy and isolated experts demonstrate that almost anything is possible, even complex living donor hepatectomy. LLR appears to offer patients real benefits when it is done well. Surgeons who perform LLR should be experienced in either open liver surgery and have laparoscopic skills or be trained in laparoscopic liver surgery. They should report their results and consider randomized trials to prove its advantages.
AcknowledgmentsOther Section
- Introduction
- Background
- Definitions
- Patient selection—start with the easy ones
- Instrumentation
- Anesthesia & pneumoperitoneum
- Bleeding
- Individual operations
- Evidence
- Conclusions
- Acknowledgments
- Footnote
- References
Funding: None.
FootnoteOther Section
- Introduction
- Background
- Definitions
- Patient selection—start with the easy ones
- Instrumentation
- Anesthesia & pneumoperitoneum
- Bleeding
- Individual operations
- Evidence
- Conclusions
- Acknowledgments
- Footnote
- References
Provenance and Peer Review: This article was commissioned by the Guest Editor (H. Leon Pachter) for the series “Laparoscopic Surgery of the Liver and Spleen” published in Laparoscopic Surgery. The article has undergone external peer review.
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ls.2020.02.02). The series “Laparoscopic Surgery of the Liver and Spleen” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
ReferencesOther Section
- Introduction
- Background
- Definitions
- Patient selection—start with the easy ones
- Instrumentation
- Anesthesia & pneumoperitoneum
- Bleeding
- Individual operations
- Evidence
- Conclusions
- Acknowledgments
- Footnote
- References
- Fortner JG, MacLean BJ, Kim DK, et al. The seventies evolution in liver surgery for cancer. Cancer 1981;47:2162-6. [Crossref] [PubMed]
- Rau HG, Meyer G, Cohnert TU, et al. Laparoscopic liver resection with the water-jet dissector. Surg Endosc 1995;9:1009-12. [Crossref] [PubMed]
- Hüscher CG, Lirici MM, Chiodini S. Laparoscopic liver resections. Semin Laparosc Surg 1998;5:204-10. [PubMed]
- Suh K, Hong S, Choi G, et al. Pure Laparoscopic Donor Hepatectomy Based On Korean Multicenter Experience. Am J Transplant 2019;19:513.
- Lewin JW, O’Rourke NA, Chiow AKH, et al. Long-term survival in laparoscopic vs open resection for colorectal liver metastases: inverse probability of treatment weighting using propensity scores. HPB 2016;18:183-91. [Crossref] [PubMed]
- Fretland ÅA, Dagenborg VJ, Bjørnelv GMW, et al. Laparoscopic Versus Open Resection for Colorectal Liver Metastases: The OSLO-COMET Randomized Controlled Trial. Ann Surg 2018;267:199-207. [Crossref] [PubMed]
- Strasberg SM, Belghiti J, Clavien PA, et al. The Brisbane 2000 Terminology of Liver Anatomy and Resections. HPB 2000;2:333-39. [Crossref]
- Kaneko H, Takagi S, Shiba T. Laparoscopic partial hepatectomy and left lateral segmentectomy: Technique and results of a clinical series.(Clinical report). Surgery 1996;120:468-75. [Crossref] [PubMed]
- Descottes B, Lachachi F, Sodji M, et al. Early experience with laparoscopic approach for solid liver tumors: initial 16 cases. Ann Surg 2000;232:641-5. [Crossref] [PubMed]
- Cherqui D, Husson E, Hammoud R, et al. Laparoscopic liver resections: a feasibility study in 30 patients. Ann Surg 2000;232:753-62. [Crossref] [PubMed]
- Gigot JF, Glineur D, Santiago Azagra J, et al. Laparoscopic liver resection for malignant liver tumors: preliminary results of a multicenter European study. Ann Surg 2002;236:90-7. [Crossref] [PubMed]
- Cherqui D. Laparoscopic liver resection. Br J Surg 2003;90:644-6. [Crossref] [PubMed]
- O’Rourke N, Fielding G. Laparoscopic right hepatectomy: surgical technique. J Gastrointest Surg 2004;8:213-6. [Crossref] [PubMed]
- Nguyen KT, Gamblin CT, Geller DA. World Review of Laparoscopic Liver Resection—2,804 Patients. Ann Surg 2009;250:831-41. [Crossref] [PubMed]
- Ciria R, Cherqui D, Geller DA, et al. Comparative Short-term Benefits of Laparoscopic Liver Resection: 9000 Cases and Climbing. Ann Surg 2016;263:761-77. [Crossref] [PubMed]
- Buell JF, Cherqui D, Geller DA, et al. The international position on laparoscopic liver surgery: The Louisville Statement, 2008. Ann Surg 2009;250:825-30. [Crossref] [PubMed]
- Cho JY, Han HS, Wakabayashi G, et al. Practical guidelines for performing laparoscopic liver resection based on the second international laparoscopic liver consensus conference. Surg Oncol 2018;27:A5-9. [Crossref] [PubMed]
- Cherqui D, Wakabayashi G, Geller DA, et al. The need for organization of laparoscopic liver resection. J Hepatobiliary Pancreat Sci 2016;23:665-7. [Crossref] [PubMed]
- Geller D. Laparoscopic Liver Resection of HCC in Childs B/C Cirrhotic patients. Proceedings of The 2nd World Congress of the International Laparoscopic Liver Society; 2019 May 9-11; Tokyo, Japan.
- Tanaka S, Kawaguchi Y, Kubo S, et al. Validation of index-based IWATE criteria as an improved difficulty scoring system for laparoscopic liver resection. Surgery 2019;165:731-40. [Crossref] [PubMed]
- Sultana A, Nightingale P, Marudanayagam R, et al. Evaluating the learning curve for laparoscopic liver resection: a comparative study between standard and learning curve CUSUM. HPB 2019;21:1505-12. [Crossref] [PubMed]
- Wakabayashi G, Cherqui D, Geller DA, et al. Recommendations for laparoscopic liver resection: a report from the second international consensus conference held in Morioka. Ann Surg 2015;261:619-29. [PubMed]
- Abe Y. Use of Energy Devices to Control Bleeding and bile leakage in Laparoscopic Liver Surgery. Proceedings of The 2nd World Congress of the International Laparoscopic Liver Society; 2019 May 9-11; Tokyo, Japan.
- Ferrero A, Russolillo N, Langella S, et al. Ultrasound liver map technique for laparoscopic liver resections: perioperative outcomes are not impaired by technical complexity. Updates Surg 2019;71:49-56. [Crossref] [PubMed]
- Hughes MJ, Ventham NT, Harrison EM, et al. Central venous pressure and liver resection: a systematic review and meta‐analysis. HPB 2015;17:863-71. [Crossref] [PubMed]
- Eiriksson K, Fors D, Rubertsson S, et al. High intra-abdominal pressure during experimental laparoscopic liver resection reduces bleeding but increases the risk of gas embolism. Br J Surg 2011;98:845-52. [Crossref] [PubMed]
- Hibi T, Cherqui D, Geller DA, et al. Expanding indications and regional diversity in laparoscopic liver resection unveiled by the International Survey on Technical Aspects of Laparoscopic Liver Resection (INSTALL) study. Surg Endosc 2016;30:2975-83. [Crossref] [PubMed]
- Otsuka Y, Katagiri T, Ishii J, et al. Gas embolism in laparoscopic hepatectomy: what is the optimal pneumoperitoneal pressure for laparoscopic major hepatectomy? J Hepatobiliary Pancreat Sci 2013;20:137-40. [Crossref] [PubMed]
- Kobayashi S, Honda G, Kurata M, et al. An Experimental Study on the Relationship Among Airway Pressure, Pneumoperitoneum Pressure, and Central Venous Pressure in Pure Laparoscopic Hepatectomy. Ann Surg 2016;263:1159-63. [Crossref] [PubMed]
- Tranchart H, O’Rourke N, Van Dam R, et al. Bleeding control during laparoscopic liver resection: a review of literature. J Hepatobiliary Pancreat Sci 2015;22:371-8. [Crossref] [PubMed]
- Hibi T, Cherqui D, Geller DA, et al. International Survey on Technical Aspects of Laparoscopic Liver Resection: a web-based study on the global diffusion of laparoscopic liver surgery prior to the 2nd International Consensus Conference on Laparoscopic Liver Resection in Iwate, Japan. J Hepatobiliary Pancreat Sci 2014;21:737-44. [Crossref] [PubMed]
- Chiow AKH, Lewin J, Manoharan B, et al. Intercostal and transthoracic trocars enable easier laparoscopic resection of dome liver lesions. HPB 2015;17:299-303. [Crossref] [PubMed]
- Laurenzi A, Cherqui D, Figueroa R, et al. Totally intra-corporeal Pringle maneuver during laparoscopic liver resection. HPB 2018;20:128-31. [Crossref] [PubMed]
- Yamamoto M, Katagiri S, Ariizumi SI, et al. Tips for anatomical hepatectomy for hepatocellular carcinoma by the Glissonean pedicle approach (with videos). J Hepatobiliary Pancreat Sci 2014;21:E53-6. [Crossref] [PubMed]
- Soubrane O, Schwarz L, Cauchy F, et al. A Conceptual Technique for Laparoscopic Right Hepatectomy Based on Facts and Oncologic Principles: The Caudal Approach. Ann Surg 2015;261:1226-31. [Crossref] [PubMed]
- Bryant R, Cavallucci D, O’Rourke N. The ‘Dorsal’ approach to laparoscopic major hepatectomy enables expanded indications for laparoscopic liver resection. HPB 2018;20:S267. [Crossref]
- Wakabayashi G, Cherqui D, Geller DA, et al. Laparoscopic hepatectomy is theoretically better than open hepatectomy: preparing for the 2nd International Consensus Conference on Laparoscopic Liver Resection. J Hepatobiliary Pancreat Sci 2014;21:723-31. [Crossref] [PubMed]
- Cherqui D, Soubrane O, Husson E, et al. Laparoscopic living donor hepatectomy for liver transplantation in children. Lancet 2002;359:392-6. [Crossref] [PubMed]
- Kwon CHD, Choi GS, Kim JM, et al. Laparoscopic Donor Hepatectomy for Adult Living Donor Liver Transplantation Recipients. Liver Transpl 2018;24:1545-53. [Crossref] [PubMed]
- Han HS, Cho JY, Yoon YS, et al. Total laparoscopic living donor right hepatectomy. Surg Endosc 2015;29:184. [Crossref] [PubMed]
- Allard MA, Cunha AS, Gayet B, et al. Early and Long-term Oncological Outcomes After Laparoscopic Resection for Colorectal Liver Metastases: A Propensity Score-based Analysis. Ann Surg 2015;262:794-802. [Crossref] [PubMed]
- van der Poel MJ, Barkhatov L, Fuks D, et al. Multicentre propensity score‐matched study of laparoscopic versus open repeat liver resection for colorectal liver metastases. Br J Surg 2019;106:783-9. [Crossref] [PubMed]
- Fretland ÅA, Aghayan D, Edwin B. Long-term survival after laparoscopic versus open resection for colorectal liver metastases. J Clin Oncol 2019;37:LBA3516 [Crossref]
- Takahara T, Wakabayashi G, Beppu T, et al. Long-term and perioperative outcomes of laparoscopic versus open liver resection for hepatocellular carcinoma with propensity score matching: a multi-institutional Japanese study. J Hepatobiliary Pancreat Sci 2015;22:721-7. [Crossref] [PubMed]
- El-Gendi A, El-Shafei M, El-Gendi S, et al. Laparoscopic Versus Open Hepatic Resection for Solitary Hepatocellular Carcinoma Less Than 5 cm in Cirrhotic Patients: A Randomized Controlled Study. J Laparoendosc Adv Surg Tech A 2018;28:302-10. [Crossref] [PubMed]
- van Dam RM, Wong-Lun-Hing EM, van Breukelen GJP, et al. Open versus laparoscopic left lateral hepatic sectionectomy within an enhanced recovery ERAS® programme (ORANGE II-trial): study protocol for a randomised controlled trial. Trials 2012;13:54. [Crossref] [PubMed]
Cite this article as: Brough D, O’Rourke N. Laparoscopic hepatic resection. Laparosc Surg 2020;4:18.


