Intraoperative management of spermatic cord lipomas: a systematic review
IntroductionOther Section
Groin pain is a common symptom in surgical practice (1). The symptoms often originate from a groin hernia such as a femoral or inguinal hernia, which in most cases can be diagnosed during physical examination. There might be a visible bulge in the groin area, or it can be provoked by e.g., the Valsalva manoeuvre. However, surgical exploration can reveal no hernia or unexpected findings such as inguinal lipomas (2,3). Special attention should be given to these lipomas since, if not removed, they can be the cause of repeated operations under suspicion of a recurrent hernia (4-6). Even if there is no hernia at surgical exploration, it has been hypothesized that the cord lipoma could provoke the development of a hernia by enlarging the deep ring and proximal portion of the inguinal canal (7-9).
The terms “sliding inguinal lipomas” or “spermatic cord lipomas” are being used widely and are often incorrect terms. In fact, these “lipomas” are rarely true lipomas as a true lipoma is a benign encapsulated tumour and quite a rare finding in the inguinal canal (10,11). Spermatic cord lipomas appear to originate from retroperitoneal fat, that extrudes through the internal inguinal ring and are encountered intraoperatively in 3–75% of the patients (6,8-10,12,13). Their etiology is not yet fully understood. One explanation could be that the lipoma develops from remnant gubernacular fat, which is retroperitoneal mesenchymal fat that guides the foetal testicular descent (14-16). To our knowledge, there is little research on how cord lipomas should be managed intraoperatively.
This systematic review aimed to investigate whether lipomas of the spermatic cord should be excised when found during groin hernia surgery and if a mesh should be inserted subsequently. We present the following article in accordance with the PRISMA reporting checklist (available at http://dx.doi.org/10.21037/ls-20-56).
MethodsOther Section
This systematic review was reported using the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) (17). The protocol was registered in PROSPERO (International prospective register of systematic reviews) with the registration number CRD42020162862. Eligible studies included original studies in English, Swedish, Norwegian, Danish, Spanish, and Turkish with a minimum patient cohort of n ≥5. Studies were required to include a description of inguinal lipomas as a possible operative finding in men and/or women. There was no age restriction. PubMed (1966–present), Embase (1947–present), and Cochrane Library (1996–present) were searched on November 25, 2019 with help from a research librarian. Additional relevant articles were sought using the snowball search method (18).
The following search terms were used for PubMed (and afterwards adapted to Embase and the Cochrane Library): (surgical procedures OR operations OR operation OR surgery OR surgical OR treatment OR management OR diagnosis OR therapy) AND (Lipoma [Mesh] OR lipoma OR lipomata OR sliding lipoma OR cord lipoma OR fatty tumour OR fatty tumours OR adipose tissue) AND (inguinal canal [Mesh] OR Spermatic cord OR Inguinal cord OR inguinal cords OR spermatic cords OR funicular OR inguinal rings OR inguinal ring OR inguinal canal OR inguinal canals OR round ligament).
The records from each database were gathered in an Excel spreadsheet where duplicates with the same title and abstract were removed. Eligibility screening was conducted by two reviewers independently, first by title and abstract and subsequently in full-text format. Discrepancies were resolved by consensus among the authors. All eligible studies were searched in the Retraction Watch Database on February 20, 2020, to ensure that none of them had been retracted (19).
The following data were extracted by double data entry by the first author into a spreadsheet in Excel from each eligible study: author name, year of publication, study design, number of participants, age range, sex of participants, type of operation, number of operations, number of removed lipomas, number of operated “real” hernias, stated factors associated with presence of a cord lipoma, number of patients with symptomatic and asymptomatic lipoma, number of patients with symptomatic relief after removed lipoma, results of histopathologic examination, follow-up method, follow-up period, and conclusion.
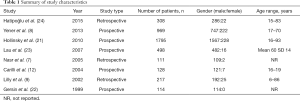
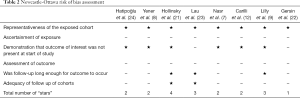
The risk of bias for observational studies was assessed using the Newcastle-Ottawa Scale (NOS) by two researchers independently (20). The NOS risk of bias tool is designed to assess non-randomized studies by awarding stars. It is possible to award a total of nine stars distributed on eight items within three main groups: selection, comparability, and outcome. Since the included studies of this review did not have any control groups, two of the eight items were left out (“selection of non-exposed cohort” and “comparability of cohorts on the basis of the design or analysis”), and therefore it was possible to give maximum six stars in total. An appropriate follow-up period was set to a minimum of 30 days, as well as an estimate of 10% for dropout where bias would be less likely to occur.
The primary outcome measures were intraoperative handling of the spermatic cord lipomas, i.e., removal or leave in place and whether to insert a mesh or not. Additional outcomes were the occurrence of spermatic cord lipomas, the occurrence of pain relief after surgical removal of spermatic cord lipomas, and the correlation between body mass index (BMI) and spermatic cord lipomas. It was decided in the author group that a meta-analysis was unfeasible since there was high heterogenicity amongst the studies.
ResultsOther Section
In total, 8 studies were included in the review. The study selection process is depicted in Figure 1. Our database search yielded 460 studies. One additional study was retrieved through a snowball search (21). After removal of duplicates, 426 studies were assessed according to the inclusion and exclusion criteria, and 8 studies were included. After a thorough search in the Retraction Watch Database, none of the included studies were found to be retracted.
Of the eight included studies, five were prospective cohort studies (8,12,21-23) and three were retrospective cohort studies (7,9,24). There were no randomized controlled trials. The accumulated patient cohort from the eight studies consisted of 4,140 patients, who were selected for operation under the suspicion of having a groin hernia. Of these, 87% were male and 13% were female with age ranging from 6–93 years. Summary of study characteristics is shown in Table 1. The total number of operated groins were higher than the patient cohort, since some patients were operated for bilateral groin hernias. In total, 4,752 groins were operated. The type of operation was either open or laparoscopic repair.
Full table
The risk of bias assessment in the included studies is presented in Table 2. The lowest ranking study received one star (22). Four studies received two stars (7,8,12,24), two studies received three stars (9,23), and one study received four stars (21). None of the studies received stars in the categories “ascertainment of exposure” or “assessment of outcome”, as they did not present from where they obtained their data on patients. Only two studies obtained stars in the category “adequacy of follow up of cohorts” (21,23), due to a lack of reporting in the rest of the studies.
Full table
The cord lipomas were defined as “fatty tissue lying in the inguinal canal, which is separable from the surrounding cord structures and distinct from the fatty tissue accompanying the testicular vessels” (8,12). Five studies described the lipomas as originating from retroperitoneal fat that herniates into the inguinal canal (7-9,23,24). Two studies did not give any definition of cord lipomas (21,22), while two studies vaguely described what cord lipomas are but without a clear definition (7,24).
Surgical removal of cord lipoma
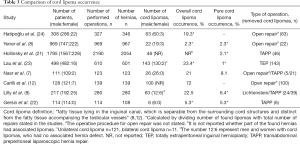
Table 3 shows whether the lipomas were found during open or laparoscopic exploration. The operation technique was described in all studies performing laparoscopic operations. Four performed transabdominal preperitoneal (TAPP) repair (7,9,21,22) and one study performed total extraperitoneal (TEP) repair (23). In three of the studies performing TAPP repair, they described that the cord lipomas were reduced and resected (9,21,22). In another study, the cord lipomas were dissected free of the cord but left in the preperitoneal space (7). In four studies using laparoscopy (7,9,22,23) a mesh was inserted, also when a cord lipoma was the only finding, i.e., no hernia. The fifth study using laparoscopy also inserted mesh at operations, but it is unclear whether it was also inserted when a lipoma was the only finding (21). Open repair was performed in five studies (7-9,12,24). One of them described that surgery was performed in a “Lichtenstein fashion” (9). Cord lipomas were resected with or without peritoneal sac in two studies performing open operation (8,12), while one study only resected cord lipomas that had no relation to the peritoneal sac and with a minimum size of 1 cm × 1 cm (24). The rest of the studies did not report a definitive size of the fat in the inguinal canal for it to be recognized as a cord lipoma. A detailed operation technique was otherwise not described in the studies performing open operations.
Full table
Occurrence of cord lipomas
Table 3 compares the total amount of operated patients in each study with the number of hernias found at exploration, and the number of cord lipomas found. Furthermore, it shows the male:female ratio of cord lipomas. In total, 469 lipomas were found in the accumulated patient cohort. When calculating the occurrence of cord lipomas, one study was not included (21). This study defined all protrusions in the inguinal region as “hernias”. The study reported 46 cord lipomas without a peritoneal defect, but it was not stated if there were any lipomas in relation to the 2,054 hernias found during surgery. Therefore, the number of lipomas and number of repairs of this study were not included in the calculation of occurrence. Thus, 423 lipomas in 2,562 groins were equivalent to 17% of operated groins. Of the 423 lipomas, 61 lipomas had no connection to a hernia sac, yielding a 2.4% occurrence for “pure” cord lipomas. Six studies included patients who were suspected of having hernias (7,9,21-24). The remaining two studies only included patients diagnosed with indirect inguinal hernias, but at operation several patients were found to have pantaloon or direct hernias besides their lipomas (8,12).
Table 4 gives an overview of the number of lipomas found with and without a detected hernia sac. Five studies identified cord lipomas in patients who had a hernia defect (7,9,12,23,24), and six studies identified lipomas without a detected hernia sac (7-9,21-23).

Full table
Pain resolution
Cord lipomas were removed both when they were found related to a hernia sac and without a hernia sac. In four studies (8,9,21,22), a total of 80 patients were symptomatic and had no hernia sac in relation to the lipoma, see Table 4. Description of pain resolution for 14/80 patients were not reported in one study (8). Of the remaining 66 patients, 63 (95%) had full symptomatic resolution postoperatively. Two patients had improvement and one patient continued to have groin pain (9). In two studies, 12 asymptomatic patients had no detected hernia sac, but on physical examination, they had a palpable bulge, which turned out to be cord lipomas (8,9).
Risk factors associated with presence of cord lipomas
Three studies investigated the correlation between the development of cord lipomas and BMI, body weight, and the size of the hernia defect (12,23,24). The average BMI in patients with lipomas for each of the three studies were 25.7, 23.8, and 26.7 compared with that of the patients with no detected lipomas being 24.6, 22.7, and 25.8, respectively (12,23,24). In two of the studies, there were significant correlations between presence of lipoma and higher BMI, P=0.023 and P=0.048 (12,23). One study found no significant correlation between BMI and presence of cord lipomas, P >0.05 (24). The incidence of cord lipoma compared with the size of the defect in all three studies showed that a larger defect was significantly associated with the risk of having a cord lipoma, P<0.05, P=0.038, and P<0.005 (12,23,24). Two of the studies compared the incidence of cord lipoma with Type II and IIIb hernias of the Nyhus classification (12,24). One study investigated if comorbidities, such as hypertension, diabetes mellitus, chronic smoking etc. were implicated in the development of cord lipomas, but none of them were predictive of cord lipomas (23).
DiscussionOther Section
This study indicates that spermatic cord lipomas are a relatively frequent finding in patients receiving surgical treatment for inguinal hernias. The cord lipomas were found in relation to hernia sacs or as an incidental finding with no relation to a hernia sac. Despite the latter occurring at a lower frequency, cord lipomas with no hernia sac are an important preoperative differential diagnosis to inguinal hernias. The included studies found that most patients, where the only pathologic finding was cord lipomas, had symptomatic relief after surgical removal/reduction of the cord lipoma. This advocates that lipomas found during groin hernia surgery should be resected as it is not known with certainty if the preoperative symptoms arise from a hernia or a lipoma. Although many studies inserted a mesh after removal of a cord lipoma, the literature does not allow firm conclusions whether a mesh should be inserted or not.
This study had several strengths. To our knowledge, this is the first review that investigates whether spermatic cord lipomas should be resected when found during surgery. The search strategy was developed with help from a research librarian, and a total of three databases were searched. Furthermore, our study had limited language bias, as two authors with a collective comprehension of five languages screened title, abstract, and full text independently. One limitation to this study was the few published studies on the subject, and that there have not been made any randomized clinical trials. Risk of bias within the included studies showed high risk (median two stars out of six). Mainly because it was decided mutually not to assign any stars in the two categories: “Ascertainment of exposure” and “Assessment of outcome”. The included studies had no description of these two categories. All cord lipomas that were found within the eight included studies were excised or reduced. Unfortunately, only three of the studies reported on the patients’ symptoms pre- and postoperatively, after their cord lipomas were removed. Furthermore, five studies did not describe follow-up method or period (7,8,12,22,24). Finally, from the available studies we were not able to determine whether a mesh should be inserted if the only intraoperative finding was a lipoma (no hernia present).
In this systematic review, we found that spermatic cord lipomas can be the cause of clinical symptoms that resemble symptoms of a hernia. Removal of lipomas seems to relieve symptoms in the vast majority of patients. Whether mesh should be used for cord lipomas is not yet known and a randomized trial on this subject is needed. Based on our findings, it is reasonable to conclude that all lipomas found during groin hernia operations should be excised or reduced to the extra-peritoneal space.
AcknowledgmentsOther Section
Funding: None.
FootnoteOther Section
Provenance and Peer Review: This article was commissioned by the Guest Editor (Jacob Rosenberg) for the series “Hernia Surgery” published in Laparoscopic Surgery. The article has undergone external peer review.
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at http://dx.doi.org/10.21037/ls-20-56
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ls-20-56). The series “Hernia Surgery” was commissioned by the editorial office without any funding or sponsorship. Dr. Jacob Rosenberg served as the unpaid Guest Editor of the series and serves as an unpaid editorial board member of Laparoscopic Surgery from Feb 2020 to Jan 2022. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
ReferencesOther Section
- LeBlanc KE, LeBlanc LL, LeBlanc KA. Inguinal hernias: diagnosis and management. Am Fam Physician 2013;87:844-8. [PubMed]
- Chang YT, Huang CJ, Hsieh JS, et al. Giant lipoma of spermatic cord mimcs irreducible inguinal hernia: a case report. Kaohsiung J Med Sci 2004;20:247-9. [Crossref] [PubMed]
- Ballas K, Kontoulis T, Skouras C, et al. Unusual findings in inguinal hernia surgery: report of 6 rare cases. Hippokratia 2009;13:169-71. [PubMed]
- Niebuhr H, Kockerling F. Surgical risk factors for recurrence in inguinal hernia repair - a review of the literature. Innov Surg Sci 2017;2:53-9. [Crossref] [PubMed]
- Lau H. Recurrence following endoscopic extraperitoneal inguinal hernioplasty. Hernia 2007;11:415-8. [Crossref] [PubMed]
- Sarosi Jr GA, Ben-David K. Recurrent inguinal and femoral hernia. UpToDate [Last updated 05 September 2019, accessed 16 March 2020]. Available online: https://www.uptodate.com/contents/recurrent-inguinal-and-femoral-hernia
- Nasr AO, Tormey S, Walsh TN. Lipoma of the cord and round ligament: an overlooked diagnosis? Hernia 2005;9:245-7. [Crossref] [PubMed]
- Yener O, Demir M, Yigitbasi R, et al. Missed lipoma of the spermatic cord. Prague Med Rep 2013;114:5-8. [Crossref] [PubMed]
- Lilly MC, Arregui ME. Lipomas of the cord and round ligament. Ann Surg 2002;235:586-90. [Crossref] [PubMed]
- Fataar S. CT of inguinal canal lipomas and fat-containing inguinal hernias. J Med Imaging Radiat Oncol 2011;55:485-92. [Crossref] [PubMed]
- Smereczynski A, Kolaczyk K. Differential diagnosis of fat-containing lesions in the inguinal canal using ultrasound. J Ultrason 2019;19:222-7. [Crossref] [PubMed]
- Carilli S, Alper A, Emre A. Inguinal cord lipomas. Hernia 2004;8:252-4. [Crossref] [PubMed]
- Fawcett AN, Rooney PS. Inguinal cord lipoma. Br J Surg 1997;84:1169. [PubMed]
- Heller CA, Marucci DD, Dunn T, et al. Inguinal canal "lipoma". Clin Anat 2002;15:280-5. [Crossref] [PubMed]
- Revzin MV, Ersahin D, Israel GM, et al. US of the inguinal canal: comprehensive review of pathologic processes with CT and MR imaging correlation. Radiographics 2016;36:2028-48. [Crossref] [PubMed]
- Favorito LA, Costa SF, Julio-Junior HR, et al. The importance of the gubernaculum in testicular migration during the human fetal period. Int Braz J Urol 2014;40:722-9. [Crossref] [PubMed]
- Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analysis: the PRISMA statement. J Clin Epidemiol 2009;62:1006-12. [Crossref] [PubMed]
- Greenhalgh T, Peacock R. Effectiveness and efficiency of search methods in systematic reviews of complex evidence: audit of primary sources. BMJ 2005;331:1064-5. [Crossref] [PubMed]
- Didier E, Guaspare-Cartron C. The new watchdogs' vision of science: a roundtable with Ivan Oransky (Retraction Watch) and Brandon Stell (PubPeer). Soc Stud Sci 2018;48:165-7. [Crossref] [PubMed]
- Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 2010;25:603-5. [Crossref] [PubMed]
- Hollinsky C, Sandberg S. Clinically diagnosed groin hernias without a peritoneal sac at laparoscopy—what to do? Am J Surg 2010;199:730-5. [Crossref] [PubMed]
- Gersin KS, Heniford BT, Garcia-Ruiz A, et al. Missed lipoma of the spermatic cord. A pitfall of transabdominal preperitoneal laparoscopic hernia repair. Surg Endosc 1999;13:585-7. [Crossref] [PubMed]
- Lau H, Loong F, Yuen WK, et al. Management of herniated retroperitoneal adipose tissue during endoscopic extraperitoneal inguinal hernioplasty. Surg Endosc 2007;21:1612-6. [Crossref] [PubMed]
- Hatipoğlu S, Kapan S. İnguinal herni tamirinde spermatik kord ve round ligamanı lipomlarına yaklaşım. Med J Bakirkoy 2015;11:109-15. [Crossref]
Cite this article as: Piga E, Gülen S, Zetner D, Andresen K, Rosenberg J. Intraoperative management of spermatic cord lipomas: a systematic review. Laparosc Surg 2021;5:24.