Long-terms results in terms of QoL after laparoscopic Nissen fundoplication: a literature review
Introduction
Surgical management of gastroesophageal reflux disease (GERD) focuses on restoring a physiologic equivalent to the normal lower esophageal sphincter (LES). A variety of antireflux procedures have been proposed for the treatment of the GERD. It was the 1956 when Rudolph Nissen described the original fundoplication and, since that time, many variations and modifications have been described, and the same named procedure may be performed differently by different surgeons (1). A common modification is a 360 degree fundic wrap without division of the short gastric vessels (Nissen-Rossetti), even if most surgeons, especially in USA, prefer to divide the short gastric vessels in order to obtain a greater freedom mobilization and reduced concern about torque on the fundoplication (2).
Minimally invasive approach could be considered as the gold standard in the surgical treatment of GERD because it has been shown to be safe, associated to a shorter hospital stays and recuperative times and to improve non only symptoms (3-5) but also QoL (6,7).
In many series, Nissen fundoplication has been found superior to other antireflux procedures, with an improvement in symptoms in a percentage ranging from 85% up to 90% (8), moreover, other studies show that, in some selected groups, such as patients who experience unrelieved heartburn by PPI, Nissen’s intervention is significantly superior in improving symptoms compared to medical therapy (9).
The way to measure the success of the fundoplication procedure may not be so obvious and simple. Some patients continue to have residual or recurrent symptoms (retching, gagging, vomiting) and the difficulties are even greater when a physician has to decide if such symptoms are a result of residual disease, of a recurrent disease if the procedure failed, or a completely different underlying disease for which fundoplication was not indicated. Another important topic is the way to assess the symptoms persistence or recurrence after surgery (10). Numerous studies over the years have evaluated both the short- and long-term efficacy of the surgical treatment of GERD and the outcome in terms of quality of life (QoL) for patients undergoing this type of surgery. QoL, in fact, has been suggested to be the most relevant parameter in order to assess and monitor the long-term outcome in patients who underwent surgery for GERD (11).
The purpose of this literary review is to evaluate results and QoL after minimally invasive Nissen or Nissen-Rossetti fundoplication with a peculiar attention to surgical outcomes on a long-term follow-up.
Methods
Eligibility criteria
The authors considered as eligible all human trials conducted on adults’ patients that reported results on Nissen and Nissen-Rossetti fundoplication whose outcomes were of interest and were retrievable. We considered studies that reported perioperative results such as complications, mortality or conversion rates, and follow-up on Nissen and Nissen-Rossetti fundoplication. Exclusion criteria were studies with a pediatric population, that not reported interesting outcome (such as the absence of QoL evaluation), with an incomplete outcome data or in the form of reviews, editorials, letters, conference abstracts and expert opinions.
Literature search
A literature search of trials available in the electronic databases (Medline, Scopus and Web of Science) was performed considering the period February 2010 - February 2020. The following keywords were used: “Nissen”, “Nissen-Rossetti”, “fundoplication”, “laparoscopic fundoplication”, “laparoscopic”, “quality of life”, “follow-up”.
Study selection and data collection
Titles and abstracts were evaluated by 2 authors in a blinded manner and disagreements were resolved by discussion with the senior author. The same procedure was performed considering the full texts of trials.
Data extraction
Data were collected from the abstract, main manuscript, tables, supplementary material, or graphs. In the evaluation of the trials, authors extracted patient characteristics, technical characteristics, perioperative outcomes and results of follow-up. Only the information available in the full text article of the trials were reported.
Outcome measures included general results after Nissen and Nissen-Rossetti fundoplication, such as surgical re-interventions, 30-day or in-hospital morbidity and mortality, long-term follow-up results according to the QoL score used in the selected studies.
Results
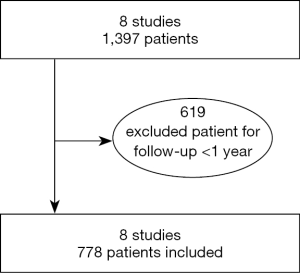
Eight studies (9,11-17) were included in our literature review. Studies of major interest and considered for literature review were published between 2012 and 2020 (Figure 1).
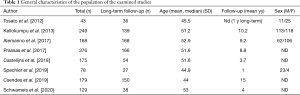
A total of 1,397 patients were considered in all selected studies (minimum 43–maximum 376), while patients submitted to a follow-up ≥1 year were in total 778 (minimum 27–maximum 168). Short gastric vessels were divided in five of the examined studies (435 patients of 778). Crural repair was performed in 7 studies, while in 1 study this data is not reported (27 patients of 778). The general description of the examined studies and the general characteristics of the population of the examined studies are reported respectively in Tables 1,2.
Full table
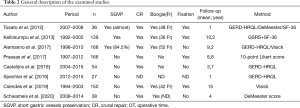
Full table
Only in two studies, authors reported a convertion from laparoscopic to open intervention, while in 5 studied is reported the rate of post-operative complications that varies from 3.6% to 14.8%. In three studies, authors refers the necessity of a re-do operation and only in one study is reported a case of perioperative death. The conversion, the reoperation rate and perioperative death of the selected studies are reported in Table 3.
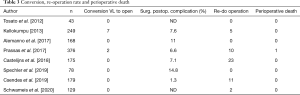
Full table
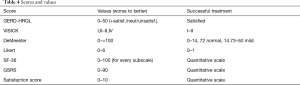
The follow-up ranged between 1 and 15 years and the QoL of patients at the end of follow-up was assessed with different scores and values: GERD-HRQL, VISICK, DeMeester, Likert, SF-36, GSRS and a Satisfaction Score. In Table 4 are reported the score and values of each score and how the score could consider the treatment as a successful.
Full table
One of the considered studies reports a long-term follow-up at 1 year, out of a total of 4 years of follow-up, as the assessment of the QoL was examined only 1 year after the intervention (9).
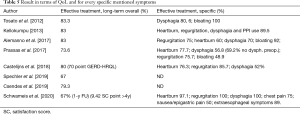
In terms of QoL, patients enrolled in the selected studies have an overall effective treatment in a percentage variable from 67% to 83.3%. Results in terms of QoL and for every specific mentioned symptoms are reported in Table 5.
Full table
Discussion
Laparoscopic Nissen fundoplication is considered as the surgical procedure of choice for managing GERD, is able, in fact, to perform an antireflux barrier in the cardia region and is able to control the typical symptoms of GERD in a high percentage of cases at long-term follow-up (9).
Many authors reported different methods in order to evaluate the QoL of patients submitted to surgery for GERD. GERD-HRQL includes 10 questions with scores between 0 and 5 for each question, and an additional question which evaluates the patient’s satisfaction with his/her current condition. Visick score measures QoL based on the presentation and severity of symptoms: (I) no symptoms, resolved; (II) mild occasional symptoms easily controlled, improved; (III) mild symptoms not controlled, unchanged; (IV) not improved, worsened (8). DeMeester and Jonson score are based on 6 variables: number of reflux episodes, maximal reflux duration, number of episodes that lasts more than 5 minutes, total percentage of time with pH <4 for the total monitoring, and with pH <4 in an upright position and supine position, respectively. There’s a simplified formula: Scoring value = [(X−A) / SD]+1. X detection value, A mean value, and SD standard deviation for each variable.
The composite score of DeMeester can be obtained by adding the scores based on each of the 6 components, where a score >14.72 is to be considered abnormal, 14.72–50 is considered as mild GERD, 51–100 is considered as moderate GERD, and >100 is considered as severe GERD (10). Likert scale is a score that can be composed of various number of domains (from five to ten and more). Each of these domains has a score ranging from 0 to 5, where: 0, no symptoms; 1, symptoms noticeable but not bothersome; 2, symptoms noticeable and bothersome, but not every day; 3, symptoms bothersome every day; 4, symptoms that affect daily life; 5, symptoms incapacitating (unable to perform daily activities) (18). SF-36 is a score that evaluate 8 domains of health-related QoL using 36 items: physical function, bodily pain, role limitation-physical, vitality, general health, social function, role limitation-emotional, mental health (19). GSRS contains fifteen items, each rated on a 7-point Likert scale from no to very severe symptoms or discomfort. The 15 GSRS items breaks down into 5 scales: abdominal pain (abdominal pain, hunger pains and nausea); reflux symptoms (heartburn and acid regurgitation), diarrhoea syndrome (diarrhoea, loose stools and urgent need for defecation), indigestion syndrome (borborygmus, abdominal distension, eructation and increased flatus) and constipation syndrome (constipation, hard stools and feeling of incomplete evacuation). The scores are calculated by taking the mean of the items completed within an individual scale, with higher scores indicating greater severity of symptoms (20,21). The satisfaction score is a quantitative score based on a subjective scale ranging from 0 to 10 (17).
In the study performed by Tosato et al. in 2012 (11), 36 patients were submitted to laparoscopic Nissen-Rossetti fundoplication for symptomatic GERD. All patients were evaluated with SF-36 and GERD-HQRL questionnaires. No post-operative death occurred and no re-intervention was needed. At 6 months 63.8% of patients were satisfied by the surgical results and at 1 year, the 83.3% of patients. Moreover, authors underline that at 6 and 12 months, no patients reported dysphagia. Authors concludes the study asserting that Nissen-Rossetti fundoplication is a safe and effective surgical procedure for the treatment of GERD, resulting in an improvement in QoL. In the study performed by Kellokumpu et al. in 2013 (12), 249 patients underwent laparoscopic Nissen Fundoplication. In 3 patients there were major intraoperative complications (1 distal esophageal perforation, 1 small fundic perforation, 1 pleural empyema in a patient with oesophageal injury), no death occurred. In 2.4% of patients it was necessary a conversion from laparoscopy to open surgery. Overall 30-day morbidity was 7.6%. One hundred and thirty-nine patients with a median follow-up of 10.2 years were available for a long-term evaluation. Eighty-three percent of patients rated their operation a success. In a study conducted in our centre (11), 168 patients underwent laparoscopic surgery for GERD. No conversion from laparoscopic to open surgery. There were 3 intraoperative complications (bleeding). No perioperative mortality was observed. Examining the trend of the VISICK and GERD-HRQL score throughout the years authors noticed an increase (worsening) of both scores, but it was only significant in the VISICK, after the first 5 years. At the end of the study (median follow-up 110±3 months), the number of unsatisfied patients according to the VISICK score (32%) was higher than the one obtained with the GERD-HRQL questionnaire (18%). In the study conducted by Prassas et al. (14), 376 patients underwent laparoscopic Nissen fundoplication. In 2 patients was necessary a conversion to open surgery due to a splenic laceration. The 30-day mortality rate was 0.27%. Thirty-day post-operative morbidity rate was 6.6%. At long-term follow-up (8.8 years), 166 patients were enrolled. One hundred twenty patients (73.6%) reported a subjective improvement of their QoL. In the study performed by Castelijns et al. (15), 231 patients were submitted to laparoscopic Nissen fundoplication. For follow-up a total of 169 patients returned the questionnaire. Authors found a complication rate of 7.1% (perforation of the stomach, bleeding, opening of the pleura). The median overall QoL score was 70 at mean follow-up of 3.7 years. There was no difference in terms of QoL among patients with a follow-up longer than 5 years (115 patients) compared with patients with follow-up of <5 years (54 patients). Twenty-three patients underwent reoperation during follow-up due to persistent dysphagia and recurrent heartburn. Mean QoL was 62.7 for patients that not require reoperation compared to 53.1 for patients that require reoperation. In the randomized trial of medical versus Surgical Treatment conducted by Spechler et al. (9), 27 patients were randomly assigned to receive surgical treatment. At 12 months, treatment success (>50% of improvement in the GERD-HRQL score) occurred in 18 of 27 patients (67%) of the surgery group. The incidence of treatment success of patients submitted to surgery was significantly superior to that submitted to medical therapy. In the study conducted by Csendes et al. (16), 179 patients were submitted to laparoscopic Nissen Fundoplication and 150 submitted to late objective evaluation of 15 years. Authors reported no operative mortality, 2 mild complications and no conversion to open surgery. In 79.3% of patients a success of treatment was observed according to the grade I and II of VISICK scale. In the study published by Schwameis et al. (17), 75 patients were evaluated. Long-term follow-up was examined only on 38 of the 75 patients evaluated. Authors evaluated the 1-year treatment success defined as a 50% or greater improvement in GERD-HRQL score that occurred in 67% of the surgical group compared to 28% in the active medical group and 12% in the control medical group.
One major issue in long-term follow-up of patients submitted to operations is the dropout phenomenon, which is mainly due to their usually poor compliance to go to the outpatient clinic, especially in case of asymptomatic subjects. However, which method should be used in the historical interview to verify the persistence or relapse of GERD symptoms is still being debated and many different scores have been used by different authors.
Among all the scores used, some are non-specifically related to the QoL, since the symptoms related to GERD significantly contribute to decrease the patients QoL. Others more specifically, instead, refer to the changes in disease related symptoms. Many data suggest a possible recurrence of the symptoms after surgery in a long follow-up period, however, the majority of QoL scores seem to be important in selecting patients who need to be instrumentally examined.
Nissen-Rossetti fundoplication could be considered as a safe and effective surgical procedure for the treatment of GERD, resulting in an improvement in QoL. The level of satisfaction and QoL obtained in selected studies were comparable with reported standards and the residual symptoms after anti-reflux surgery were easily controlled. Although a large variety of disease-specific QoL questionnaires are reported in literature in order to evaluate patients affected by GERD, there is still a lack of a recognized standard scale.
Conclusions
Laparoscopic Nissen fundoplication is a safe and effective surgical procedure that could control the typical symptoms of GERD and improve patient’s QoL, but new-onset symptoms could affect postoperative well-being. In conclusion, for a closer evaluation of the benefits of the operation, it is necessary to identify new questionnaires or standardized methods that evaluate the symptom spectrum of GERD both preoperatively and postoperatively.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Andrea Balla) for the series “Minimally Invasive Approach for the Treatment of Gastro-esophageal Reflux Disease” published in Laparoscopic Surgery. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ls-20-64). The series “Minimally Invasive Approach for the Treatment of Gastro-esophageal Reflux Disease” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Nissen R. Eine einfache Operation zur Beeinflussung der Refluxoesophagitis A simple operation for control of reflux esophagitis. Schweiz Med Wochenschr 1956;86:590-2. [PubMed]
- DeMeester TR, Bonavina L, Albertucci M. Nissen fundoplication for gastroesophageal reflux disease. Evaluation of primary repair in 100 consecutive patients. Ann Surg 1986;204:9-20. [Crossref] [PubMed]
- Trus TL, Laycock WS, Branum G, et al. Intermediate follow-up of laparoscopic antireflux surgery. Am J Surg 1996;171:32-5. [Crossref] [PubMed]
- Peters JH, Heimbucher J, Kauer WK, et al. Clinical and physiologic comparison of laparoscopic and open Nissen fundoplication. J Am Coll Surg 1995;180:385-93. [PubMed]
- Rattner DW, Brooks DC. Patient satisfaction following laparoscopic and open antireflux surgery. Arch Surg 1995;130:289-93; discussion 293-4. [Crossref] [PubMed]
- Velanovich V. Comparison of symptomatic and quality of life outcomes of laparoscopic versus open antireflux surgery. Surgery 1999;126:782-8; discussion 788-9. [Crossref] [PubMed]
- Trus TL, Laycock WS, Waring JP, et al. Improvement in quality of life measures after laparoscopic antireflux surgery. Ann Surg 1999;229:331-6. [Crossref] [PubMed]
- Ellis FH Jr. The Nissen fundoplication. Ann Thorac Surg 1992;54:1231-5. [Crossref] [PubMed]
- Spechler SJ, Hunter JG, Jones KM, et al. Randomized Trial of Medical versus Surgical Treatment for Refractory Heartburn. N Engl J Med 2019;381:1513-23. [Crossref] [PubMed]
- Dent J, Armstrong D, Delaney B, et al. Symptom evaluation in reflux disease: workshop background, processes, terminology, recommendations, and discussion outputs. Gut 2004;53 Suppl 4:iv1-iv24. [Crossref] [PubMed]
- Alemanno G, Bergamini C, Prosperi P, et al. A long-term evaluation of the quality of life after laparoscopic Nissen-Rossetti anti-reflux surgery. J Minim Access Surg 2017;13:208-14. [Crossref] [PubMed]
- Tosato F, Marano S, Mattacchione S, et al. Quality of life after Nissen-Rossetti fundoplication. Surg Laparosc Endosc Percutan Tech 2012;22:205-9. [Crossref] [PubMed]
- Kellokumpu I, Voutilainen M, Haglund C, et al. Quality of life following laparoscopic Nissen fundoplication: assessing short-term and long-term outcomes. World J Gastroenterol 2013;19:3810-8. [Crossref] [PubMed]
- Prassas D, Krieg A, Rolfs TM, et al. Long-term outcome of laparoscopic Nissen fundoplication in a regional hospital setting. Int J Surg 2017;46:75-8. [Crossref] [PubMed]
- Castelijns PSS, Ponten JEH, Vd Poll MCG, et al. Quality of life after Nissen fundoplication in patients with gastroesophageal reflux disease: Comparison between long- and short-term follow-up. J Minim Access Surg 2018;14:213-20. [Crossref] [PubMed]
- Csendes A, Orellana O, Cuneo N, et al. Long-term (15-year) objective evaluation of 150 patients after laparoscopic Nissen fundoplication. Surgery 2019;166:886-94. [Crossref] [PubMed]
- Schwameis K, Oh D, Green KM, et al. Clinical outcome after laparoscopic Nissen fundoplication in patients with GERD and PPI refractory heartburn. Dis Esophagus 2020;33:doz099. [Crossref] [PubMed]
- Velanovich V. Comparison of generic (SF-36) vs. disease-specific (GERD-HRQL) quality-of-life scales for gastroesophageal reflux disease. J Gastrointest Surg 1998;2:141-5. [Crossref] [PubMed]
- Hays RD, Sherbourne CD, Mazel RM. The RAND 36-Item Health Survey 1.0. Health Econ 1993;2:217-27. [Crossref] [PubMed]
- Revicki DA, Wood M, Wiklund I, et al. Reliability and validity of the Gastrointestinal Symptom Rating Scale in patients with gastroesophageal reflux disease. Qual Life Res 1998;7:75-83. [Crossref] [PubMed]
- Dimenäs E, Carlsson G, Glise H, et al. Relevance of norm values as part of the documentation of quality of life instruments for use in upper gastrointestinal disease. Scand J Gastroenterol Suppl 1996;221:8-13. [Crossref] [PubMed]
Cite this article as: Alemanno G, Bottari A, Giordano A, Prosperi P. Long-terms results in terms of QoL after laparoscopic Nissen fundoplication: a literature review. Laparosc Surg 2021;5:9.