
Totally extraperitoneal repair using lightweight mesh and fixation with fibrin adhesive has a low reoperation rate—a register based cohort study
Introduction
Minimally invasive inguinal hernia surgery with totally extraperitoneal (TEP) repair is recognised as a safe and cost-effective method. It has been shown to have shorter recovery time and less postoperative pain than the open anterior mesh approach (1). The recurrence rates have dropped after 1999, due to improved technical performance (2,3). TEP is still associated with a long learning curve and the results are depending on the quality of the surgeon´s technique and caseload per surgeon (1,4,5). Register based studies have pointed out that the reoperation rate differed significantly between the genders undergoing laparo-endoscopic surgery for primary hernias with an advantage for females (6-8).
It is not clear; however, which mesh is the best choice in TEP repair. Regarding the type of mesh, not only large direct hernia, one should consider if fixation is necessary, to reduce the recurrence rate.
The use of macroporous lightweight mesh (LWM) in open inguinal hernia surgery reduces postoperative pain, increases patient comfort and provides better quality-of-life compared to heavyweight mesh (HWM) (9). The International Endohernia Society (IEHS) could not find evidence suggesting better postoperative quality-of-life using LWM in laparo-endoscopic hernia surgery (2,3). A Swedish register based study has also shown an increased risk of reoperations for recurrences with use of LWM in TEP repair (10).
It is believed that mesh with reduced density of material i.e., polypropylene carry an increased risk of displacement and bulging due to their lesser foreign-body response and decreasing collagen deposition, and may also contribute to the increased risk for recurrence (1,10). An increase in mesh size to cover all hernia orifices with adequate overlap and enhanced the adhesion between the mesh and the abdominal wall with an atraumatic fixation may aid in the prevention of hernia recurrence when using macroporous LWM.
Hernia Surge Guidelines have recommended fixation of large medial hernia (M3, EHS classification) only, preferably using an atraumatic technique such as fibrin adhesive, to minimise the risk for acute postoperative pain (1). The benefit of atraumatic fixation is that it eliminates the risk for any undue ‘harm’ that can occur with traumatic fixation of the mesh, such as the use of ‘tacks’. Fixation with clips or tacks increases the risk for neurovascular damage or injury to surrounding structures, including the bladder (1).
The aim of this study was to analyse our reoperation rate after TEP as a proxy for recurrences. A secondary aim was to investigate the 30-day postoperative complication rate. We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/ls-20-120).
Methods
The Swedish Hernia Register (SHR) was founded in 1992. All patients are recorded with a personal identity number unique for each Swedish citizen. This means that regardless of where in Sweden any reoperation is carried out, this can be traced in SHR. Mora hospital has a caption area of 300,000 inhabitants concerning hernia repairs and was one of the first eight units to participate in the register. Today, the SHR has over 95 participating units covering more than 97% of all groin hernia repairs performed in Sweden (11).
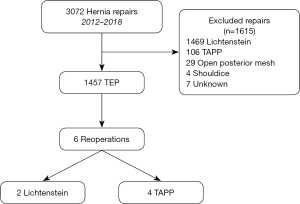
Data were retrieved from SHR on all patients who had undergone TEP at our unit between January 2012 and December 2018. Informed consent was taken from all the patients in connection with operation registrations in SHR. Our tailored approach in inguinal hernia repair based on the guidelines are reported in Figure 1. All patients were followed up 30-day postoperatively by going through their medical files.
Recurrent hernia was classified as an SHR-registered reoperation on the ipsilateral side after TEP performed between January 2012 and December 2019. A retrospective review of reoperation cases was undertaken to identify any possible contributing risk factors.
The study has been reviewed by the Swedish Ethics Review Authority dnr 2020-02858. The study was conducted in accordance with the Declaration of Helsinki (revised 2013) (12).
Materials
A macroporous LWM (<50 g/m2) was used throughout the study period. All mesh information are extracted from the register. Repairs were initially performed using polypropylene (PP) composite mesh Ultrapro™ (weight >28 g/m2, pore size >3 mm). From January 2017 this was changed to Ultrapro Advanced ™ (weight 39 g/m2, pore size 2.7 mm) (Johnson & Johnson International, Belgium). Approximately 10% of hernias were covered with a 100% PP mesh; Soft mesh ™ (weight 43.7 g/m2, pore size 2.5 mm) (Bard Limited, UK).
A mesh size of 15 cm × 15 cm was cut to 12 cm × 15 cm (breadth × length) and fixed with the stripes horizontally using 2 mL Tisseel ™ (Baxter Medical AB, Kista, Sweden), applied with a Duplospray MIS applicator® (Baxter, Healthcare Corporation, Deerfield, USA).
The adhesive was applied by holding the applicator 1–2 cm from the tissue and the mesh, starting from the lower lateral border to medial, then the lateral side of the mesh and thereafter applying an evenly distributed layer at the upper border and around the defects. (Video 1).
Results
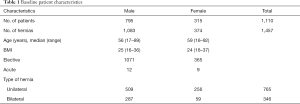
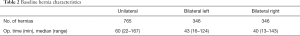
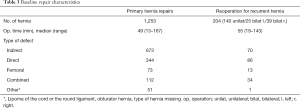
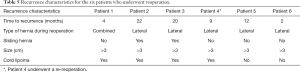
A total of 1,457 TEP procedures were performed between January 2012 and December 2018 (Figure 2). All repairs during the period were performed by five hernia specialists or surgical trainees under supervision. The majority of repairs were elective primary hernias in men but 204 (14%) were operations for a recurrent hernia (Tables 1-3). Three hundred and seventy-four patients (28%) were women in this cohort. Bilateral repairs accounted for 47% of all repairs and 32% were performed on female hernias (Tables 1-3). There was no difference in BMI between the genders but the females were slightly older. A reoperation has a longer operating time, but most repairs took just under one hour (Tables 1-3). Median postoperative follow-up time was 36 months, with a minimum of one year. Six (0.4%) males underwent a reoperation for recurrence after TEP, all had lateral hernias with defects more than 3 centimetres, identical to the original location. One male had a combined hernia (Tables 4,5). Five patients had risk factors for recurrent inguinal hernia; two with sliding hernia (patient 2 and 3), one with obesity (patient 1), patient 4 had an anterior repair before TEP and patient 1 and 6 indicate insufficient surgical technique because early recurrence and long operation time during the TEP procedure (Tables 4,5).
Full table
Full table
Full table

Full table
Full table
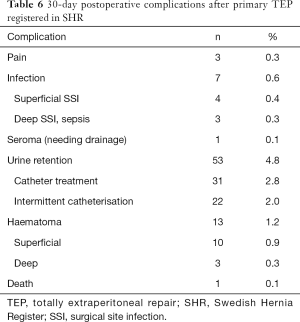
The most common 30-day postoperative complication was urinary retention in 39 males and 14 females. Mean age was higher for those who were affected by urine retention (70 year for males and 76 for females) than the rest of the cohort. Nine females needed catheter treatment all in connection with an emergency hernia repair. None of the patients with a deep haematoma needed reoperation, but one got a drain peroperative. We had no mesh infections. An 82-year-old man died of an acute myocardial infarction 21 days after a bilateral TEP repair (Table 6).
Full table
Discussion
The present register based cohort of patients operated at Mora Hospital, clearly depicts a low incidence of reoperation (0.4%) for TEP using a macroporous LWM with fibrin adhesive fixation. All our recurrences were diagnosed within 24 months after surgery, which is consistent with figures in the current literature (13). Population-based registry studies have high external validity, reflecting real-life data and the clinical routines as they are practised in the community at large, but the validity of the result will depend on the quality of data recorded. Therefore, it is very important to have standardised routines for registration. At our unit an assistant nurse together with the surgeon are doing all the registrations online during the hernia operations to reduce errors and missed data. One limitation is that SHR only registered patients undergoing hernia surgery and not everyone with a recurrence, another issue is that no planned postoperative examinations are performed.
According to the SHR Annual Report 2018 (11), the overall reoperation rate after TEP repair in Sweden between 1999 and 2018 was 3.6%. It should be noted, however, that this figure does not consider mesh type, fixation or re-do surgery.
A study performed by Melkemichel et al. (10) based on 13,839 TEP repairs in Sweden registered in the SHR between 2005 and 2013, found a recurrence rate of 4.0% in the LWM group and 3.2% in the HWM group. Furthermore, the reoperation rate in the fixated HWM group and the fixated LMW group were comparable (3.6% versus 3.8%). Our recurrence rate is lower and one reason could be our standardised technique.
Female hernia repairs normally account for 9–11% of all procedures, but in this TEP series, the percentage was considerably higher (26%), partly due to referrals from other hospitals outside the catchment area of Mora Hospital. No one of these females got a reoperation under the study period. In our unit 2018, 97% of female and 62% of male patients underwent TEP or transabdominal preperitoneal repair (TAPP) compared to 75% women and 30% men in the rest of the country (14). This statement indicates that it takes time to implement recommendations from the guidelines. Various studies have shown that women have a significantly higher reoperation rate than men, especially after an open anterior mesh repair due to missed femoral hernias. This underlines the advantage of minimal invasive posterior repair, which visualises all hernia orifices (1,7,15).
Unfortunately, recurrent inguinal hernia repair has a higher risk for further recurrence (16). However, in this series only one male in the recurrent hernia repair group (0.5%) needed a re-reoperation (Tables 1-4).
All the recurrences were found at reoperation to have the same anatomical origin as the primary hernia, which is consistent with the current literature (17,18). In general, medial hernias are more prone to recur than lateral hernias mainly due to collagen weakness, inadequate mesh coverage and caudal mesh release (1,10,19). Nevertheless, in this cohort no direct hernia recurrences were registered, probably due to sufficient medial mesh overlap together with fibrin adhesive fixation. It must be pointed out, however, that adequate fixation does not compensate for inadequate dissection and/or too small a meshes, regardless of the method used.
A possible reason for the lateral recurrences in this cohort may have been forgotten cord lipomas, sliding hernias, insufficient dissection and/or overlap laterally at the primary repair. It is possible that with large lateral hernias such as sliding hernias, a tailored approach with a mesh width greater than 15 cm is necessary to overcome the impact of the abdominal wall pressure on the mesh with subsequent risk for migration.
Leaving a cord lipoma at the primary repair may lead to a persisting lump in the groin that is difficult to distinguish from a true hernia. At worst, this could lead to an unnecessary procedure for supposed recurrence (20).
A deep haematoma was only seen in three patients (0.3%). This low figure was possibly the result of both meticulous dissection and the haemostatic effect of Tisseel™. Katkhouda et al. (21) concluded that fibrin adhesive reduces bleeding and haematoma in the Retzius space associated with blunt dissection, especially in patients with a coagulopathy. In TEP surgery, Tisseel can be used for haemostasis in places where you do not want to use diathermy as in the “Triangle of pain”.
TEP has a long learning curve because of the anatomical complexity and the narrow operation field, and it is estimated that 50–100 procedures are required before self-sufficiency is achieved (1,4,5). Young surgeons today “grow up with a laparoscope in their hand” which in the long round will affect the learning curve. A logarithmic function model predicted that 37–39 cases were needed to overcome the learning curve for TEP (22). Nevertheless, in this cohort only one of the repairs resulting in a re-reoperation was performed by a trainee. This confirms that TEP is a safe surgical technique at a unit using a standardised procedure where there is a system for quality assurance that involves trainees and specialists alike. The present data show that if dissection is undertaken meticulously and a mesh of sufficient size fixated with fibrin adhesive is used, any disadvantage of LWM can be surmounted, giving recurrence rates equivalent or lower to those using HWM in TEP.
Conclusions
In the setting of a teaching hospital, using a standardised procedure where quality is assured, TEP using macroporous LWM and fixation with fibrin adhesive has a very low recurrence rate and few serious postoperative complications.
Acknowledgments
Lars-Göran Larsson, M.D. Department of Surgery, Mora Hospital, Sweden for filming and editing the video. Data manager Oscar Öhman register centre north SHR, Umeå, Sweden for data support. Professor AJ Sheen Department of Surgery, Manchester University NHS Foundation Trust, Manchester, M13 9WL, UK and Peter Cox, Norrköping, Sweden for skilful linguistic revision.
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Jacob Rosenberg) for the series “Hernia Surgery” published in Laparoscopic Surgery. The article has undergone external peer review.
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/ls-20-120
Peer Review File: Available at http://dx.doi.org/10.21037/ls-20-120
Data Sharing Statement: Available at http://dx.doi.org/10.21037/ls-20-120
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ls-20-120). The series “Hernia Surgery” was commissioned by the editorial office without any funding or sponsorship. Dr. Österberg reports personal fees from Baxter, outside the submitted work. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (2013 revision) and informed consent was obtained from all the patients prior to registration in the SHR. The study was approved by the Swedish Ethics Review Authority dnr 2020-02858.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- The Hernia Surge Group. International guidelines for groin hernia management. Hernia 2018;22:1-165. [Crossref] [PubMed]
- Bittner R, Arregui ME, Bisgaard T, et al. Guidelines for laparoscopic (TAPP) and endoscopic (TEP) treatment of inguinal hernia Surg Endosc 2011;25:2773-843. [International Endohernia Society (IEHS)]. [Crossref] [PubMed]
- Bittner R, Montgomery MA, Arregui A, et al. Update of Guidelines on laparoscopic (TAPP) and endoscopic (TEP) treatment of inguinal hernia. Surg Endosc 2015;29:289-321. [Crossref] [PubMed]
- Köckerling F, Sheen AJ, Berrevoet F, et al. The reality of general surgery training and increased complexity of abdominal wall hernia surgery. Hernia 2019;23:1081-91. [Crossref] [PubMed]
- Poelman MM, van der Heuvel B, Deelder JD, et al. EAES consensus development conference on endoscopic repair of groin hernias. Surg Endosc 2013;27:3505-19. [Crossref] [PubMed]
- Lundström KJ, Holmberg H, Montgomery A, et al. Patient-reported rates of chronic pain and recurrence after groin hernia repair. Br J Surg 2018;105:106-12. [Crossref] [PubMed]
- Nilsson H, Holmberg H, Nordin P. Groin hernia repair in women - A nationwide register study. Am J Surg 2018;216:274-9. [Crossref] [PubMed]
- Bay-Nielsen M, Kehlet H. Inguinal herniorrhaphy in women. Hernia 2006;10:30-3. [Crossref] [PubMed]
- Bringman S, Wollert J, Österberg J, et al. Three-year results of a randomized clinical trial of lightweight or standard polypropylene mesh in Lichtenstein repair of primary inguinal hernia. Br J Surg 2006;93:1056-9. [Crossref] [PubMed]
- Melkemichel M, Bringman S, Widhe B. Lower recurrence rate with heavyweight mesh compared to lightweight mesh in laparoscopic totally extra-peritoneal (TEP) repair of groin hernia: a nationwide population-based register study. Hernia 2018;22:989-97. [Crossref] [PubMed]
- Annual report 2018, Swedish Hernia Register. Available online: http://www.svensktbrackregister.se
- World Medical Association Declaration of Helsinki. ethical principles for medical research involving human subjects. JAMA 2013;310:2191-4. [Crossref] [PubMed]
- Magnusson N, Nordin P, Hedberg M, et al. The time profile of groin hernia recurrences. Hernia 2010;14:341-4. [Crossref] [PubMed]
- Mora Clinical Report 2018, Swedish Hernia Register. Available online: http://www.svensktbrackregister.se
- Koch A, Edwards A, Haapaniemi S, et al. Prospective evaluation of 6895 groin hernia repairs in women. Br J Surg 2005;92:1553-8. [Crossref] [PubMed]
- Sevonius D, Gunnarsson U, Nordin P, et al. Recurrent groin hernia surgery. Br J Surg 2011;98:1489-94. [Crossref] [PubMed]
- Burcharth J, Andresen K, Pommergaard KC, et al. Recurrence patterns of direct and indirect inguinal hernias in a nationwide population in Denmark. Surgery 2014;155:173-7. [Crossref] [PubMed]
- Bringman S, Holmberg H, Österberg J. Location of recurrent groin hernias at TEP after Lichtenstein repair: a study based on the Swedish Hernia Register. Hernia 2016;20:387-91. [Crossref] [PubMed]
- Öberg S, Jessen ML, Andresen K, et al. Technical details and finding during a second Lichtenstein repair or a second laparoscopic repair in the same groin: a study based on medical records. Hernia 2021;25:149-57. [Crossref] [PubMed]
- Köckerling F, Schug-Pass C. Spermatic Cord Lipoma-A Review of the Literature. Front Surg 2020;7:39. [Crossref] [PubMed]
- Katkhouda N, Mavor E, Friedlander MH, et al. Use of fibrin sealant for prostheticmesh fixation in laparoscopic extraperitoneal inguinal hernia repair. Ann Surg 2001;233:18-25. [Crossref] [PubMed]
- Kwon OC, Baik YH, Oh MG, et al. The Learning Curve for Laparoscopic Totally Extraperitoneal Herniorrhaphy by Logarithmic Function. J Minim Invasive Surg 2016;19:126-9. [Crossref]
Cite this article as: Melén CJ, Sandblom G, Österberg J. Totally extraperitoneal repair using lightweight mesh and fixation with fibrin adhesive has a low reoperation rate—a register based cohort study. Laparosc Surg 2021;5:18.



