
A rare case report of an appendiceal abscess with a pneumatocele and direct extension into an anterior abdominal wall abscess
Introduction
Acute appendicitis is a common surgical condition with a lifetime risk of 7–8% (1). It remains the most common indication for emergency surgery (2) and is managed laparoscopically with low morbidity and mortality. The clinical presentation ranges from acute inflammation to abscess and perforation. There are reports of perforation into the retroperitoneum causing abscesses of the psoas muscle, right perinephric space, lumbar triangles, groin and thigh (3,4).
Perforation associated with an Amyand hernia has been documented in the literature (5), as well as an abdominal wall abscess leading to an enterocutaneous fistula (6-9). On rare occasions, these infections have caused necrotizing fasciitis of the abdominal wall musculature (10-14). The surgical management has varied and has included percutaneous drainage with an interval appendectomy, laparoscopic appendectomy, or a laparotomy and surgical debridement of the infected area. We present a case of perforated appendicitis manifesting as an anterior abdominal wall abscess. This was initially managed with intravenous antibiotics and a percutaneous drain, followed by an interval appendectomy. There have been eight published reports in the English literature of an appendix abscess with direct extension onto the anterior abdominal wall (6-13). The majority of published reports to date have documented a retroperitoneal appendix perforation. The abdominal wall abscess forms through a lateral extension of the pus that tracks on to the anterior abdominal wall. We present the following case in accordance with the CARE reporting checklist (available at https://ls.amegroups.com/article/view/10.21037/ls-21-14/rc).
Case presentation
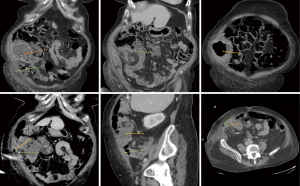
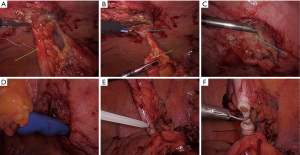
A 77-year-old woman presented to the acute care surgical team with abdominal pain, nausea and vomiting. She was clinically stable with no signs of pyrexia, chills or rigors. Abdominal examination revealed a swelling over her right iliac fossa. The swelling was fluctuant and the margins poorly defined, with no signs of surgical crepitus. There were clinical signs of rebound tenderness and guarding. Significant laboratory investigations included a leukocytosis and an increased C-reactive protein. Her medical history was significant for dementia and she resided in a care home. She had no previous abdominal surgery. A computerized tomography (CT) scan showed an intra-abdominal abscess with extension into the right anterior abdominal wall (Figure 1A). It originated from an acutely inflamed ruptured appendix with an appendicolith in situ (Figure 1B-1D). Medical treatment was initiated with intravenous antibiotics and opiate analgesia. Antibiotics included a third-generation cephalosporin (ceftriaxone) and metronidazole. The patient was subsequently discussed with an interventional radiologist. A percutaneous abdominal drain was inserted and 100 milliliters of purulent fluid drained. Culture and sensitivity grew a multitude of organisms. The drain was accidentally removed after three days and a repeat CT scan showed complete resolution of the abscess including the anterior abdominal wall component (Figure 1E,1F). The patient made an uneventful recovery and was discharged home on a course of oral antibiotics that included a second-generation cephalosporin (cephazolin) and metronidazole. Three weeks later during routine follow-up, the patient had physiologically improved with a clinically soft abdomen and no palpable masses. She had no fever, chills or rigors since her discharge. After an extensive discussion with the patient and her family, she signed an informed consent for an elective laparoscopic appendectomy. At laparoscopy, the caecum and appendix were adherent to the anterior abdominal wall. Mobilization of the caecum showed the appendix entering into an abdominal wall defect. This was thought to be the source of the previous abdominal wall abscess (Figure 2A,2B). The appendicolith was still in situ and adherent to the anterior abdominal wall (Figure 2C). The appendix was mobilized and a standard laparoscopic appendectomy performed (Figure 2D-2F). The patient made an uneventful recovery and was discharged home after three days. Pathology confirmed an appendicitis with no features of malignancy. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
While acute appendicitis remains a common surgical presentation, the atypical presentation of an appendiceal abscess can pose a challenge in diagnosis and appropriate surgical intervention. Perforation can occur in up to 30% of patients with acute appendicitis (15) and carries an increased risk of morbidity and mortality (16). CT is helpful in identifying the etiology and extent of the abdominal wall abscess. It’s superior sensitivity and specificity to ultrasound or MRI (17) is useful in planning appropriate therapy in the setting of organ perforation. Percutaneous abscess drainage is well-established as a safe, effective option in clinically stable patients (18,19). Initial conservative management followed by an interval appendectomy avoids the increased risk of perioperative complications associated with surgery in an inflamed surgical field (18,20). This can reduce the overall length of the hospital stay, thereby decreasing the financial burden to the patient and the healthcare system (20). The role of an interval appendectomy has been widely discussed and advocated for in certain patient populations due to the increased risk of recurrence, associated malignancy or inflammatory bowel disease (18). In our case, controversy arose as to whether our patient needed an interval appendectomy, as she had made a complete physiologic recovery to her acute pathological condition. Interval appendectomy is no longer performed routinely after an episode of acute organ infection (20).
After an extensive discussion with her family, it was decided to proceed with surgery. Her dementia precluded her ability to be a good historian and her age increased the risk of an appendicular or colonic malignancy. The presence of an appendicolith also contributed to the surgical algorithm as a possible nidus for a recurrent abscess (Figure 2C). She will also undergo an elective colonoscopy as part of her colonic surveillance for malignancy given the association between appendicitis and colonic malignancy in elderly patients. This case is unusual as the abdominal wall abscess was formed via a direct anterior route through the anterior abdominal wall. Most published case reports of an abdominal wall abscess involving a ruptured appendix have demonstrated a retroperitoneal abscess with tracking of the pus laterally onto the anterior abdominal wall. The etiology for direct extension of the abscess remains nebulous. It is thought that the appendicolith could have been a contributing factor through erosion of the posterior sheath of the abdominal wall, in addition to the anterior position of the appendix. A unique feature of this case is the presence of a large abdominal wall pneumatocele (Figure 1C,1E,1F). This is a unique presentation and we believe the first time it has been documented.
Conclusions
This case report illustrates an atypical presentation of perforated appendicitis in a patient with an anterior abdominal wall abscess and pneumatocele. It was successfully managed with intravenous antibiotics, percutaneous abscess drainage and an interval appendectomy.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://ls.amegroups.com/article/view/10.21037/ls-21-14/rc
Peer Review File: Available at https://ls.amegroups.com/article/view/10.21037/ls-21-14/prf
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://ls.amegroups.com/article/view/10.21037/ls-21-14/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Bhangu A, Søreide K, Di Saverio S, et al. Acute appendicitis: modern understanding of pathogenesis, diagnosis, and management. Lancet 2015;386:1278-87. Erratum in: Lancet 2017;390:1736. [Crossref] [PubMed]
- Sammalkorpi HE, Mentula P, Leppäniemi A. A new adult appendicitis score improves diagnostic accuracy of acute appendicitis--a prospective study. BMC Gastroenterol 2014;14:114. [Crossref] [PubMed]
- Souza IMAG, Nunes DAA, Massuqueto CMG, et al. Complicated acute appendicitis presenting as an abscess in the abdominal wall in an elderly patient: A case report. Int J Surg Case Rep 2017;41:5-8. [Crossref] [PubMed]
- Hsieh CH, Wang YC, Yang HR, et al. Retroperitoneal abscess resulting from perforated acute appendicitis: analysis of its management and outcome. Surg Today 2007;37:762-7. [Crossref] [PubMed]
- Ahmed K, Hakim S, Suliman AM, et al. Acute appendicitis presenting as an abdominal wall abscess: A case report. Int J Surg Case Rep 2017;35:37-40. [Crossref] [PubMed]
- Beaumont O, Miller R, Guy R. Atypical presentation of appendicitis. BMJ Case Rep 2016;2016:bcr2016217293. [Crossref] [PubMed]
- Gockel I, Jäger F, Shah S, et al. Appendicitis necessitatis: appendicitis perforating the abdominal wall. Chirurg 2007;78:840-2. [Crossref] [PubMed]
- Liu LP, Sheng XP, Shuai TK, et al. Helicobacter pylori promotes invasion and metastasis of gastric cancer by enhancing heparanase expression. World J Gastroenterol 2021;27:3138-41. [Crossref] [PubMed]
- Singal R, Gupta S, Mittal A, et al. Appendico-cutaneous fistula presenting as a large wound: a rare phenomenon-brief review. Acta Med Indones 2012;44:53-6. [PubMed]
- Beerle C, Gelpke H, Breitenstein S, et al. Complicated acute appendicitis presenting as a rapidly progressive soft tissue infection of the abdominal wall: a case report. J Med Case Rep 2016;10:331. [Crossref] [PubMed]
- Chen CW, Hsiao CW, Wu CC, et al. Necrotizing fasciitis due to acute perforated appendicitis: case report. J Emerg Med 2010;39:178-80. [Crossref] [PubMed]
- Huang ZH, Chiu YC, Ho LL, et al. Acute appendicitis complicated with necrotizing fasciitis in a patient with adult-onset Still's disease: A case report. Medicine (Baltimore) 2018;97:e9794. [Crossref] [PubMed]
- Romanoff A, Freed J, Heimann T. A case report of necrotizing fasciitis of the abdominal wall: A rare, life-threatening complication of a common disease process. Int J Surg Case Rep 2016;28:355-6. [Crossref] [PubMed]
- Taif S, Alrawi A. Missed acute appendicitis presenting as necrotising fasciitis of the thigh. BMJ Case Rep 2014;2014:bcr2014204247. [Crossref] [PubMed]
- Barrett ML, Hines AL, Andrews RM. Trends in Rates of Perforated Appendix, 2001–2010. HCUP Statistical Brief #159. Rockville, MD, USA: Agency for Healthcare Research and Quality, 2013.
- Peltokallio P, Tykkä H. Evolution of the age distribution and mortality of acute appendicitis. Arch Surg 1981;116:153-6. [Crossref] [PubMed]
- Dahabreh IJ, Adam GP, Halladay CW, Steele DW, Daiello LA, Wieland LS, Zgodic A, Smith BT, Herliczek TW, Shah N, Trikalinos TA. Diagnosis of Right Lower Quadrant Pain and Suspected Acute Appendicitis. Rockville, MD, USA: Agency for Healthcare Research and Quality, 2015.
- Andersson RE, Petzold MG. Nonsurgical treatment of appendiceal abscess or phlegmon: a systematic review and meta-analysis. Ann Surg 2007;246:741-8. [Crossref] [PubMed]
- Cantasdemir M, Kara B, Cebi D, et al. Computed tomography-guided percutaneous catheter drainage of primary and secondary iliopsoas abscesses. Clin Radiol 2003;58:811-5. [Crossref] [PubMed]
- Guida E, Pederiva F, Grazia MD, et al. Perforated appendix with abscess: Immediate or interval appendectomy? Some examples to explain our choice. Int J Surg Case Rep 2015;12:15-8. [Crossref] [PubMed]
Cite this article as: Pon K, Pillay Y. A rare case report of an appendiceal abscess with a pneumatocele and direct extension into an anterior abdominal wall abscess. Laparosc Surg 2022;6:7.


