
Gastrointestinal outcomes following transversus abdominus plane blocks in laparoscopic colorectal surgery: a systematic review
Introduction
The use of enhanced recovery pathways (ERP) is becoming increasingly common in hospitals worldwide as institutions place more emphasis on cost reduction and improvement of patient outcomes in the perioperative setting. ERP classically incorporates five evidence-based aspects: firstly, patient education, setting of expectations, and follow up; secondly, preservation of gastrointestinal function by limiting fasting time, and use of prophylactic antiemetics; thirdly, minimisation of invasive procedures such as bowel prep, surgical drains and nasogastric tubes, and where possible, preference for non-invasive surgical techniques and avoidance of open surgery; fourth, optimisation of pain control utilising analgesia initiation in the preoperative phase, and incorporation of opioid sparing agents including regional and local anaesthetic; and finally, encouragement of patient autonomy through minimisation of bladder catheterisation, intravenous fluids and sleep disruption, and emphasis on early mobilisation and breathing exercises (1).
Use of opiate-based analgesia is associated with increased post-operative nausea and vomiting (PONV), urinary retention, respiratory depression, sedation and delayed return to gut function (2,3). ERPs aim to reduce post-operative pain, thereby reducing opiate use and hastening recovery in the post-operative period through the use of non-invasive surgical techniques and multimodal analgesia incorporating local and regional anaesthetic, along with systemic non-opiate analgesia such as IV lidocaine and non-steroidal anti-inflammatory agents. Post-operative ileus is complication of particular significance due to its impact on patient recovery and length of stay (LOS) (4). Ileus is generally multifactorial and can be attributed to surgical site intestinal inflammation, associated sympathetic response to surgical intervention on the gut, and use of opioids (5). Therefore, one would imagine that sparing of opiates would have a beneficial effect on post-operative return to gut function.
A significant body of evidence exists to support the efficacy of abdominal wall nerve blocks in reducing post-operative pain and opiate requirement post abdominal surgery (6). The transversus abdominus plane (TAP) block involves the injection of local anaesthetic into the plane between the transversus abdominus and internal oblique muscles, allowing multi-dermatomal spread of local anaesthetic to nerves supplying the anterior abdominal wall (2,7). This is classically performed intraoperatively, and bupivacaine appears to be the most common local anaesthetic of choice in the literature.
ERP multimodal anaesthetic techniques such as local and regional blocks can be low cost to incorporate and have the potential to significantly decrease LOS, providing further cost reduction to institutions and patients alike (2,7). The reduction in use of opiate analgesia also has the benefit of potentially reducing or eliminating incidence of side effects such as PONV and complications such as post-operative ileus. There is increasing evidence that duration of post-operative ileus can be reduced from on average 96–120 hours to as short as 24–48 hours following laparoscopic colonic resection through the use of ERP techniques; however, the direct relationship between regional abdominal wall anaesthetic techniques and rates of ileus has not been thoroughly described (1,8). The purpose of this systematic review is to compare the rates of post-operative ileus in patients undergoing laparoscopic colorectal resection with or without use of regional nerve block analgesia in order to better understand the effect of opiate sparing regional analgesia in return of gut function. We present the following article in accordance with the PRISMA reporting checklist (available at https://ls.amegroups.com/article/view/10.21037/ls-21-22/rc).
Methods
Data sources and literature searches
To identify eligible studies, a literature review was performed using Medline/PubMed (1946) CINAHL (1981), Informit, Scopus (1970), The Cochrane Library (1951), Web of science (1965) and Embase (1974) databases, from database inception until November 2020 without language or geographic restrictions. Titles and abstracts were screened to identify relevant articles, and potentially relevant articles had their full text examined to assess eligibility using predefined inclusion and exclusion criteria. Duplicate removal was undertaken using EndNote X8. These database searches were supplemented by hand searching reference lists of included studies. Two authors undertook these searches (L.F, R.P.) on separate occasions and a consensus meeting was held during which discrepancies were resolved.
Eligibility criteria
Studies were eligible for inclusion in this review if they compared the frequency of postoperative ileus in patients with and without TAP blocks performed during laparoscopic colorectal surgery. Studies comparing TAP blocks to epidural anaesthesia were excluded. Articles were excluded if: (I) they were not written in English; (II) relevant data could not be extracted; (III) they were case reports, reviews, or letters to the editor.
Data extraction
Data were extracted from the included studies by two authors (L.F. and R.P.). Data to be extracted included year of publication, study methodology, surgical procedure, indication for surgery, type of block, timing of block, anaesthetic agent used, method of analgesia for the control group, number of cases, number of controls, number of ileus cases in each group. Discrepancies were resolved through a consensus meeting. Risk of bias for each study was assessed (L.F.) using the Cochrane Collaboration risk of bias tool.
Statistical analysis
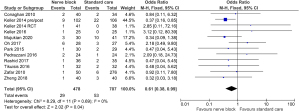
Data were analysed and extracted using the RevMan 5.3 software (the Nordic Cochrane Centre, Copenhagen, Denmark). Dichotomous outcomes were evaluated using the odds ratio (ORs) with 95% CI. The Mantel-Haenszel (M-H) random effects model was applied. Continuous outcomes were assessed using mean difference, with the inverse variance model applied. Heterogeneity was assessed using the I2 statistic. P value of less than 0.05 provided evidence of significant OR and I2. Forest plots were generated for data visualisation by the same software.
Results
Search results
An initial search identified 174 studies after the removal of duplicates (Figure 1). A total of 151 abstracts were excluded as they were irrelevant to the research question. Full text evaluation was undertaken for 23 publications, of which 18 were excluded. The most common reasons for exclusion were not reporting ileus or open surgery being performed. An additional 7 studies were identified through screening the reference lists of included studies. A total of 12 studies were ultimately included in the analysis (2,3,7,9-17).

Characteristics of included studies
The characteristics of the included studies are shown in Table 1. Five studies were randomised controlled trials, one utilised a prospective case matched design, and the remaining six were prospective non-randomised cohort studies. A total of 1,185 patients were included, including 478 patients receiving abdominal wall blocks and 707 control patients. Sample sizes ranged from 48 to 326, with a median sample size of 71. Bupivacaine was the local anaesthetic of choice in eight studies, ropivacaine in three, and levobupivacaine in one. All surgeries were laparoscopic colorectal resections. All but one study utilised patient-controlled analgesia post operatively (9).
Table 1
| Identifier | Study design | Block drug | Block group | Control group | Block technique | Timing of block |
|---|---|---|---|---|---|---|
| Conaghan 2010 | Prospective cohort | Levobupivacaine | 40 | 34 | Posterior | Post-induction pre-incision |
| Keller 2014 | Prospective cohort | Bupivacaine | 102 | 106 | Lateral | Completion of procedure |
| Keller 2014 | RCT | Bupivacaine | 41 | 38 | Lateral | Completion of procedure |
| Keller 2016 | Prospective, case-matched | Bupivacaine | 25 | 25 | Not specified | Post-induction pre-incision |
| Mujukian 2020 | Prospective cohort | Bupivacaine | 30 | 41 | Lateral | Completion of procedure, prior to extraction excision |
| Oh 2017 | RCT | Bupivacaine | 28 | 27 | Lateral | Post-induction pre-incision |
| Park 2015 | Prospective cohort | Ropivacaine | 30 | 29 | Lateral | Completion of procedure |
| Pedrazzani 2016 | Prospective cohort | Ropivacaine | 24 | 24 | Lateral | Completion of procedure |
| Rashid 2017 | RCT | Bupivacaine | 36 | 35 | Lateral | Post-induction pre-incision |
| Tikuisis 2016 | RCT | Ropivacaine | 32 | 32 | Lateral | Post-induction pre-incision |
| Zafar 2010 | Prospective cohort | Bupivacaine | 50 | 276 | Lateral | Post-induction pre-incision |
| Zheng 2018 | Prospective RCT | Ropivacaine | 40 | 40 | Lateral | Post-induction pre-incision |
RCT, randomised controlled trial.
Study quality was generally high, with the main risk of bias coming from the lack of blinding of the non-randomised controlled trials (Figure 2) (2,9,10,12-15). There was high risk of selection bias in three cohort studies, where group allocation was determined by ultrasound availability or anaesthetist preference (2,9,10). The remaining three cohort studies grouped patients by date of surgery (12,14,15).

Analysis
Twelve studies were included in statistical analysis (Figure 3) (2,3,7,9-17). A total of 82 cases of ileus were recorded, 29 in the nerve block group and 53 in the control group. Overall, there was a significant difference in the frequency of postoperative ileus between the two groups, with an odds ratio for ileus after a nerve block of 0.61 (95% CI: 0.38 to 0.99, P=0.04). Subgroup analysis of randomised controlled trials revealed no difference, with an odds ratio of 0.97 (95% CI: 0.40 to 2.38, P=0.95). Subgroup analysis was also performed for block timing, individually for blocked performed pre-incision and those at the completion of procedure. There was a statistically significant reduction in ileus frequency with blocks performed at procedure completion (OR 0.46; 95% CI: 0.25 to 0.86, P=0.01), which was not observed with pre-incisional blocks. (OR 0.95; 95% CI: 0.44 to 2.04, P=0.9).
Total opiate consumption in equivalent milligrams of morphine was reported heterogeneously, although analysis was possible for consumption during the first 24-hour period post-operatively across 5 studies involving 320 surgeries (Figure 4A) (2,3,14,16,17). This showed a significantly significant reduction in opiate use of 9.79 mg of IV morphine (95% CI: –16.98 to –2.59 mg, P≤0.01) in the nerve blockade cohort.

The frequency of PONV was reported by six studies, with 91 events recorded among 401 surgeries (Figure 4B) (2,3,7,9,11,17). While there was a trend in favour of nerve blockade, this did not reach statistically significance, with an odds ratio of 0.59 (95% CI: 0.34 to 1.01, P=0.06).
A similar trend in favour of nerve blockade was observed in the time to first bowel opening and time to first oral intake (Figure 4C,4D), but these was also statistically insignificant, with a standard mean difference of –0.55 days (95% CI: –1.22 to 0.11 days, P≤0.0002) for time to first bowel opening and –0.44 days (95% CI: –0.93 to 0.05 days, P=0.08). The data for these comparisons was limited, each only being reported in four studies (2,3,9,17).
The length of hospital stay was reported by nine studies (Figure 4E), including 754 surgeries, with a statistically significant reduction of hospital stay in the group receiving nerve blockade with a mean difference of –1.08 days (95% CI: –1.71 to –0.46 days, P≤0.01) (2,3,7,9-12,14,17).
Discussion
This systematic review aimed to explore the relationship between intra-operative TAP block and incidence of post-operative ileus. It was hypothesised that the opiate-sparing effect of regional analgesia would confer lower rates of post-operative ileus in patients undergoing laparoscopic colonic resection. This was based on a body of evidence suggesting that opiates are implicated in genesis of post-operative ileus and that regional anaesthesia has opiate sparing effect (5,7). This review identified a significant reduction in the rate of postoperative ileus with regional abdominal wall block in patients undergoing laparoscopic colonic resection. This trend was not established among the subset of randomised control trial studies, although this was likely underpowered, with only 20 cases of ileus amongst these studies.
Given the multifactorial aetiology of ileus, this reduction may not be attributable to regional anaesthesia alone, with patient, surgical and aesthetic factors all potentially playing a role. Some studies included largely (>80%) or exclusively patients receiving surgery for cancer treatment, who likely differ from other populations such as inflammatory bowel disease or diverticulosis in characteristics such as local inflammation and prior opiate use (2,3,9,16). Additionally, 5 studies excluded any patients with a history of opiate tolerance or chronic opiate use, where regional anaesthesia may be of most benefit, but again were not unified in their results, as many other factors are involved (2,3,7,16,17).
While all studies included in this review were colorectal resections, study populations differ in the type of resection, underlying pathology, and surgical technique, which may have led to confounding of these results. For example, the study by Conaghan et al. found a statistically significant reduction in opiate use only with left hemicolectomies, but not right sided surgeries. This may be explained but their surgical technique, with left sided surgeries having the resected bowel removed through a left lower quadrant incision, whereas an incision in the right upper quadrant was used for right sided resections (10). Many other studies utilised midline paraumbilical or suprapubic incisions for this same purpose, which should theoretically be covered by the area of the block (2,3,9,15-17).
Further, the pressure of peritoneal insufflation was only recorded in the study by Rashid et al., in which insufflation pressures were a standard 12 mmHg (3). As discussed by Celarier et al., reduction of laparoscopic pneumoperitoneum pressure to 7 mmHg caused a significant reduction in analgesia requirement, postoperative pain, and LOS in patients undergoing laparoscopic colectomy (18). This is thought to be a result of reduced visceral pain caused by wall tension, organ compression and bowel traction, as well as reduced referred pain caused by diaphragmatic stretch, phrenic nerve irritation and persistent gas pockets (19). It is difficult to determine whether insufflation pressure varied across the included cohort given that this parameter was not recorded in the majority of cases. While TAP blocks effectively alleviate abdominal wall pain, they do not provide coverage for visceral pain or referred pain; the pressure of insufflation is therefore a potential uncontrolled variable in this data set and represents a worthwhile area for further investigation.
The method and timing of TAP block may also have resulted in differences between studies. Five techniques of TAP block are described in the literature: Subcostal, oblique subcostal, lateral, posterior and dual TAP blocks (20,21). In the present review, only Conaghan et al. utilised a posterior TAP block, with the remainder reporting a lateral TAP block, with the exception of Keller et al. 2016 where type of block was not reported (10,13). The posterior technique involves inserting the needle through the lumbar triangle of Petit, whereas the lateral technique involves insertion of the needle between the iliac crest and costal margin in either the mid or anterior axillary line. The lateral technique is thought to provide analgesia from the midline to the midaxillary line, whereas the posterior technique may offer better analgesia to the lateral abdominal wall. This a result of the anatomy of the lateral cutaneous branches of the segmental nerves, which arise and leave the TAP posterior to the midaxillary line (20,21). Lastly, while all blocks were performed in theatre, there was divide between timing of blocks, with seven studies performing the block post-induction, pre-incision, and five providing blockade immediately following completion of the operation, prior to waking. On subgroup analysis of this data, there was a significant reduction in ileus in studies performing a completion TAP block, while no effect was observed with pre-incisional block. This may be explained by the duration of action of a single shot block lasting only approximately 6–10 hours, meaning a significant proportion of the analgesic effect may be lost from pre-incisional blocks by the time the patient leaves the recovery area (21).
A significant reduction in morphine use was identified in the blocked group, which supports the existing literature that regional anaesthesia reduces opiate consumption (6). The group receiving TAP block used on average 9.79 mg less of IV morphine compared to control groups. This figure is similar to the 10 mg IV morphine equivalents discussed by Laigaard et al. (2021) in their systematic review describing clinician-perceived minimal clinically important difference in post operative opiate use following total hip or knee arthroplasty (22). Therefore, the reduction of opiate use observed in the included studies is likely approaching the threshold of clinical importance and is not merely a statistically significant observation. This meaningful reduction in opiate use could be interpreted as indirect measure of a reduction in the total pain burden experienced by patients following colorectal resection, and may be implicated in the reduction of ileus frequency observed in this study It would be worthwhile to examine rates of post-operative ileus with and without regional anaesthetic in patients undergoing non-abdominal surgery or abdominal surgery not involving the bowel, such as gynaecological or urological procedures, in order to eliminate the inflammatory response to bowel resection as a confounding factor, in order to determine if may be the case. There currently appears to be a dearth in the literature regarding these procedures and scope exists for further studies in this area.
In addition to this, it has recently been proposed that the mechanism of fascial plane blocks such as the TAP block may be at least partly a result of systemic absorption of local anaesthetic, rather than regional anaesthesia (23). This has been noted by Tsui et al. to be an issue in the reporting of data by such studies, with only 35% presenting data about sensory change in the blocked area, rather than outcomes such as opiate consumption, of which a reduction may be the result either systemic or regional effects (24). To evaluate this effect, Lonnqvist et al. have proposed the inclusion of a third group in fascial plane block studies, to receive intravenous local anaesthetic as an additional control to placebo (25). In the present review, no included studies reported data on sensory change in the blocked area, limiting the confidence in results being attributable to the regional rather than systemic effect. Furthermore, a previous systematic review found evidence to support the use of iv lignocaine for reducing time to return to bowel function postoperatively and LOS, although they authors did not directly compare rates of ileus between intravenous and fascial plane administration (26).
While the present review did find a significant reduction in length of hospital stay (mean difference 1.08 days; 95% CI: –1.71 to –0.46 days), this was not the case for time to first bowel opening (mean difference –0.55 days; 95% CI: –1.22 to 0.11 days) and time to first oral intake (mean difference –0.44 days; 95% CI: –0.93 to 0.05 days), despite a trend in favour of TAP block. This may be due to the limited data available for analysis for these variables, being reported on in only four studies. This trend was also identified in post-operative nausea and vomiting (OR 0.64; 95% CI: 0.39 to 1.05), which is thought to be related to a reduction in opiate consumption in the test group, as opiates gave been implicated in nausea and vomiting in the post-operative period, as discussed by Park et al. and Rashid et al. (2,3).
Of the 12 studies included in this review, three different trial formats were used: five randomised control trials, six prospective non-randomised cohort studies and one prospective case match study. The inclusion of non-randomised studies increases the risk of bias within the data set. Additionally, the control groups in each of these studies were treated under different protocols, with some being placed on an ERP, and some on a standard post-operative management pathway. The definition of these protocols was not always possible to establish, and significant variability exists between ERPs at different institutions, as well as between “standard” or non-ERP post-operative protocols. Further, there was no way to establish consistency between the included studies in regard to variables such as timing of block administration, pain scoring systems and definition of post-operative complication. The small sample size limits confidence in the data.
Conclusions
Regional abdominal wall analgesia with TAP blockade has been shown to have an opioid sparing effect in the post-operative period, with a significant reduction in the rate of post-operative ileus and LOS. Additionally, performing single shot nerve blockade at the completion of surgery demonstrated a reduction in ileus that was not observed with block performed pre-incision. A trend in favour of nerve blockade was identified for time to first bowel opening, time to first oral intake and PONV, although not statistically significant. There is minimal data currently available in the literature to determine if these benefits apply to other methods of abdominal wall nerve blockade or non-colorectal surgery, and these are potential avenues for further investigation.
Acknowledgments
The authors acknowledge the contribution of Dr. Leigh White for his feedback and advice in writing this article.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at https://ls.amegroups.com/article/view/10.21037/ls-21-22/rc
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://ls.amegroups.com/article/view/10.21037/ls-21-22/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Adamina M, Kehlet H, Tomlinson GA, et al. Enhanced recovery pathways optimize health outcomes and resource utilization: a meta-analysis of randomized controlled trials in colorectal surgery. Surgery 2011;149:830-40. [Crossref] [PubMed]
- Park JS, Choi GS, Kwak KH, et al. Effect of local wound infiltration and transversus abdominis plane block on morphine use after laparoscopic colectomy: a nonrandomized, single-blind prospective study. J Surg Res 2015;195:61-6. [Crossref] [PubMed]
- Rashid A, Gorissen KJ, Ris F, et al. No benefit of ultrasound-guided transversus abdominis plane blocks over wound infiltration with local anaesthetic in elective laparoscopic colonic surgery: results of a double-blind randomized controlled trial. Colorectal Dis 2017;19:681-9. [Crossref] [PubMed]
- Tevis SE, Carchman EH, Foley EF, et al. Postoperative Ileus--More than Just Prolonged Length of Stay? J Gastrointest Surg 2015;19:1684-90. [Crossref] [PubMed]
- Kehlet H, Dahl JB. Anaesthesia, surgery, and challenges in postoperative recovery. Lancet 2003;362:1921-8. [Crossref] [PubMed]
- Zhao X, Tong Y, Ren H, et al. Transversus abdominis plane block for postoperative analgesia after laparoscopic surgery: a systematic review and meta-analysis. Int J Clin Exp Med 2014;7:2966-75. [PubMed]
- Keller DS, Ermlich BO, Schiltz N, et al. The effect of transversus abdominis plane blocks on postoperative pain in laparoscopic colorectal surgery: a prospective, randomized, double-blind trial. Dis Colon Rectum 2014;57:1290-7. [Crossref] [PubMed]
- Luckey A, Livingston E, Taché Y. Mechanisms and treatment of postoperative ileus. Arch Surg 2003;138:206-14. [Crossref] [PubMed]
- Pedrazzani C, Menestrina N, Moro M, et al. Local wound infiltration plus transversus abdominis plane (TAP) block versus local wound infiltration in laparoscopic colorectal surgery and ERAS program. Surg Endosc 2016;30:5117-25. [Crossref] [PubMed]
- Conaghan P, Maxwell-Armstrong C, Bedforth N, et al. Efficacy of transversus abdominis plane blocks in laparoscopic colorectal resections. Surg Endosc 2010;24:2480-4. [Crossref] [PubMed]
- Zheng J, Feng Z, Zhu J. Effect of preintravenous injection of parecoxib, combined with transversus abdominis plane block in strategy of enhanced recovery after radical resection of colorectal cancer. J Cancer Res Ther 2018;14:1583-8. [Crossref] [PubMed]
- Keller DS, Stulberg JJ, Lawrence JK, et al. Process control to measure process improvement in colorectal surgery: modifications to an established enhanced recovery pathway. Dis Colon Rectum 2014;57:194-200. [Crossref] [PubMed]
- Keller DS, Tahilramani RN, Flores-Gonzalez JR, et al. Pilot study of a novel pain management strategy: evaluating the impact on patient outcomes. Surg Endosc 2016;30:2192-8. [Crossref] [PubMed]
- Mujukian A, Truong A, Tran H, et al. A Standardized Multimodal Analgesia Protocol Reduces Perioperative Opioid Use in Minimally Invasive Colorectal Surgery. J Gastrointest Surg 2020;24:2286-94. [Crossref] [PubMed]
- Zafar N, Davies R, Greenslade GL, et al. The evolution of analgesia in an 'accelerated' recovery programme for resectional laparoscopic colorectal surgery with anastomosis. Colorectal Dis 2010;12:119-24. [Crossref] [PubMed]
- Oh TK, Yim J, Kim J, et al. Effects of preoperative ultrasound-guided transversus abdominis plane block on pain after laparoscopic surgery for colorectal cancer: a double-blind randomized controlled trial. Surg Endosc 2017;31:127-34. [Crossref] [PubMed]
- Tikuisis R, Miliauskas P, Lukoseviciene V, et al. Transversus abdominis plane block for postoperative pain relief after hand-assisted laparoscopic colon surgery: a randomized, placebo-controlled clinical trial. Tech Coloproctol 2016;20:835-44. [Crossref] [PubMed]
- Celarier S, Monziols S, Célérier B, et al. Low-pressure versus standard pressure laparoscopic colorectal surgery (PAROS trial): a phase III randomized controlled trial. Br J Surg 2021;108:998-1005. [Crossref] [PubMed]
- Özdemir-van Brunschot DM, van Laarhoven KC, Scheffer GJ, et al. What is the evidence for the use of low-pressure pneumoperitoneum? A systematic review. Surg Endosc 2016;30:2049-65. [Crossref] [PubMed]
- Tsai HC, Yoshida T, Chuang TY, et al. Transversus Abdominis Plane Block: An Updated Review of Anatomy and Techniques. Biomed Res Int 2017;2017:8284363. [Crossref] [PubMed]
- Chin KJ, McDonnell JG, Carvalho B, et al. Essentials of Our Current Understanding: Abdominal Wall Blocks. Reg Anesth Pain Med 2017;42:133-83. [Crossref] [PubMed]
- Laigaard J, Pedersen C, Rønsbo TN, et al. Minimal clinically important differences in randomised clinical trials on pain management after total hip and knee arthroplasty: a systematic review. Br J Anaesth 2021;126:1029-37. [Crossref] [PubMed]
- Byrne K, Smith C. Erector spinae plane block: systemic local anesthetic by proxy? Reg Anesth Pain Med 2021;46:639-40. [Crossref] [PubMed]
- Tsui BCH, Fonseca A, Munshey F, et al. The erector spinae plane (ESP) block: A pooled review of 242 cases. J Clin Anesth 2019;53:29-34. [Crossref] [PubMed]
- Lonnqvist PA, Karmakar MK, Richardson J, et al. Daring discourse: should the ESP block be renamed RIP II block? Reg Anesth Pain Med 2021;46:57-60. [Crossref] [PubMed]
- McCarthy GC, Megalla SA, Habib AS. Impact of intravenous lidocaine infusion on postoperative analgesia and recovery from surgery: a systematic review of randomized controlled trials. Drugs 2010;70:1149-63. [Crossref] [PubMed]
Cite this article as: Fairley LJ, Patane R. Gastrointestinal outcomes following transversus abdominus plane blocks in laparoscopic colorectal surgery: a systematic review. Laparosc Surg 2022;6:11.


